COVID-19: Detected change in blood vessels in the lungs
International research team with MHH participation successfully uses new X-ray technique for the first time.
Stand: 04. November 2021
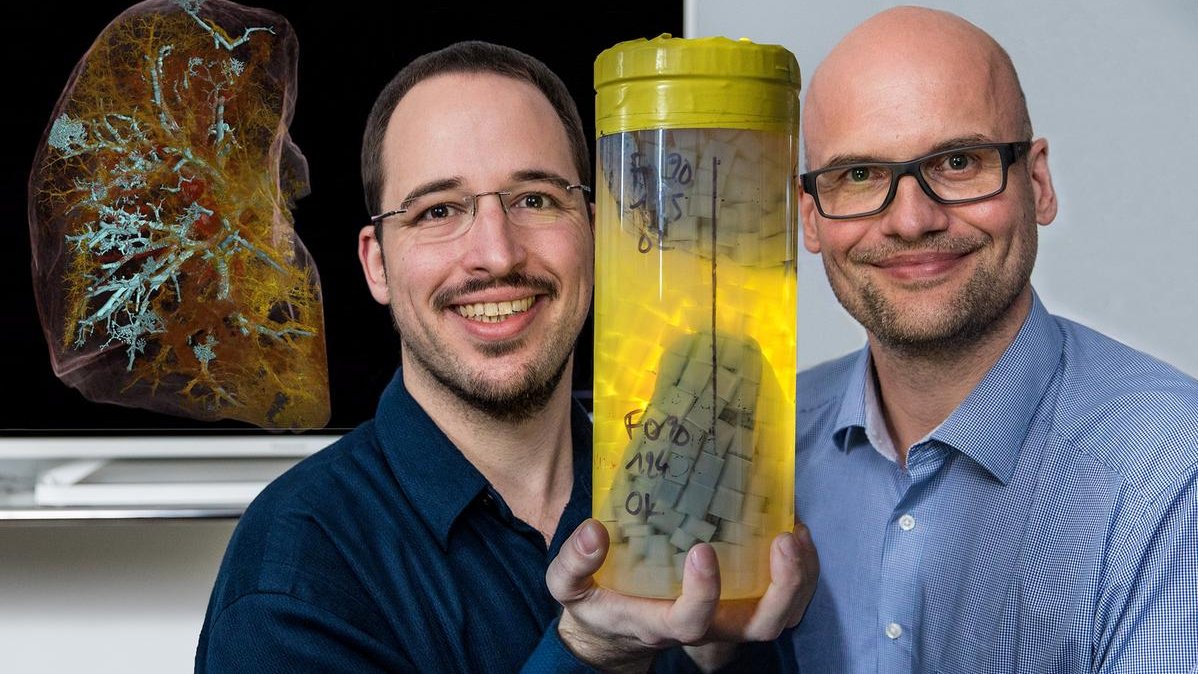
When the SARS-Cov-2 coronavirus enters the lung, it causes massive tissue damage. A characteristic consequence of the infection is, among other things, the blockage of the pulmonary vessels due to a locally excessive blood clotting. Now, an international research team led by Professor Dr. Danny Jonigk and Christopher Werlein from the Institute of Pathology at the Hannover Medical School (MHH) and PD Dr. Max Ackermann from the University Medical Center Mainz has been able to demonstrate for the first time, using a highly innovative X-ray technique in a non-destructive manner, that severe COVID-19 causes massive remodelling of the finest blood vessels by causing normally separate blood systems to join together with unusual frequency.
For this purpose, the researchers examined the lungs of a COVID-19 victim in cooperation with the European Synchrotron Research Facility (ESRF), the world's third largest particle accelerator in Grenoble, France. Thanks to the latest technology, a three-dimensional image of the complete organ could be generated for the first time using high-resolution X-rays. The work has resulted in two publications in renowned journals: The technical procedure is published in Nature Methods, the clinical application in the American Journal of Respiratory and Critical Care Medicine (Blue Journal).
HiP-CT shows an entire organ three-dimensionally without damaging it
The new X-ray technique works much like a computed tomography (CT) scan in a hospital. However, the resolution is a hundred times higher. "In the CT scan, we can show blood vessels in the millimetre range," Professor Jonigk explains. The new technology called Hierarchical Phase Contrast Tomography (HiP-CT) is able to image the finest vessels with a diameter of five micrometres - about one tenth the thickness of a hair. HiP-CT makes it possible to penetrate into the depths of the lungs and depict even the smallest structures down to individual cells. "Until now, this resolution was only possible with a microscope, but only in two dimensions and for small tissue samples," says the lung specialist. HiP-CT can do much more. With the new technique, it is possible for the first time to image an entire organ three-dimensionally and greatly magnified without damaging it. "This made it possible to examine structures that are at the limits of resolution and to gain an overview of the changes in the entire lung tissue," emphasises the pathologist.
COVID-19 leads to "short circuits" in the blood vessels of the lung
In this way, the scientists discover what seems to go wrong with COVID-19. There are two separate blood systems in the lungs - one belongs to the pulmonary circulation and is responsible for supplying oxygen to the entire body, the other supplies the lung tissue itself with the vital gas. In a healthy lung, there are sometimes a few connections between small vessels of the two systems. In the damaged COVID-19 lung, on the other hand, the two blood systems formed numerous such cross-links in many areas. "This large number of irreversible shunts acts like a wide-open sluice gate and ensures that the oxygen supply in the entire body no longer functions," explains Professor Jonigk. He suspects that the cause is a dysregulation of the lung itself, which thus tries to compensate for the lack of oxygen caused by the SARS-CoV2 infection in the short term in a kind of short-circuit reaction.
The brilliant, high-resolution technology will revolutionise medical imaging and our understanding of the structure of our bodies, says Professor Jonigk. "Now we have the ability to visualise tiny structures three-dimensionally in their proper spatial context on a large scale," he explains. The research team has already begun to create a more advanced organ atlas. In addition to the COVID-19-damaged lung, it already contains images of several healthy human organs such as the brain, lungs, heart, kidneys and spleen from deceased body donations. The pathologist is also convinced that the HiP-CT X-ray technology will provide new insights into numerous diseases, including cancer and Alzheimer's disease.
The work was done in cooperation between the MHH Institute of Pathology and, among others, the German Centre for Lung Research in Hanover (DZL Breath), University College London and the University Medical Center Mainz.
The original paper on the clinical application "The Bronchial Circulation in COVID-19 Pneumonia" can be found here, and the original paper on the technical procedure "Imaging intact human organs with local resolution of cellular structures using hierarchical phase-contrast tomography" can be found here.
Strengthening the virus defence with larch extract and more exercise

MHH study investigates the influence of prostaglandin E2 on the immune system
Stand: 24. August 2021
Not all infections with SARS-CoV-2 run the same course. Certain factors increase the risk of contracting COVID-19. Age, gender and lifestyle seem to play an important role. An international research team from the Department of Cardiology and Angiology at the Hannover Medical School (MHH) and the University of Marburg, in cooperation with the Twincore Center for Experimental and Clinical Research, a joint facility of the MHH and the Helmholtz Centre for Infection Research, has investigated why older men with a lack of exercise are particularly at risk. The focus of the work is the tissue hormone prostaglandin E2 (PGE2). In viral infections, the messenger substance suppresses the innate and learned immune system and promotes the spread of the viruses. However, there are ways to lower the level of PGE2 in the blood and improve the immune defence. This can be done with physical exercise as well as treatment with taxifolin, a naturally occurring PGE2 inhibitor derived from Siberian larch extract. The study has been published in the multidisciplinary online journal of the Public Library of Science (PLOS ONE).
COVID-19 sufferers have fewer immune cells
Our immune system can actually successfully fight off viral diseases. Two types of cells from the group of white blood cells are particularly important for this: T-cells and B-cells. T cells can directly destroy virus-infected cells, and they enable B cells to form virus-neutralising antibodies. However, PGE2 ensures that fewer of these two cell types are present to defend against SARS-CoV-2 infection. "We received lung tissue and blood samples from Belgium, Italy and from the Hannover Unified Biobank at MHH from patients severely affected by COVID-19 and found significantly elevated levels of PGE2," explain Dr Melanie Ricke-Hoch and Dr Denise Hilfiker-Kleiner, Professor of Molecular Cardiology at MHH and now Dean at the Faculty of Medicine at Philipps University Marburg. The tissue hormone throttles the production of the protein PAX5, which in turn regulates the formation and maturation of B cells. This weakens the immune system and the viruses can spread unhindered. In examinations of lung tissue samples from people who died of COVID-19, there were actually significantly fewer B cells than in healthy lungs, the scientists report.
SARS-CoV-2 stimulates further infections
The research team was also able to show that SARS-CoV-2 is partly responsible for this increased PGE2 production in the lung epithelium. Since PGE2 also reduces the number of B cells, the virus itself thus seems to ensure that the antiviral immune response is weaker. "This opens the door for secondary infections, for example, by fungi, as has already occurred frequently in India," explains Professor Hilfiker-Kleiner. Renewed infections with SARS-CoV-2 are then also possible. According to the scientist, this reinfection could be the reason why the immune reaction suddenly overshoots in severe COVID-19 courses and organ damage occurs as a result.
Taxifolin can lower PGE2 levels
However, elevated PGE2 levels also occur in non-infected people, especially in older people with inactive lifestyles. But there are drugs that can lower PGE2 levels and thus improve the immune response. One of these is called taxifolin. The substance is extracted from the wood of the larch tree and is freely available as a food supplement. In cell culture, the research team was able to prove that the plant extract acts as a PGE-2 inhibitor. "Whether this can be considered as a preventive measure for risk patients, however, must first be clarified in further studies," says Dr. Ricke-Hoch. Another option is more exercise. "We examined blood samples from healthy seniors who completed twelve months of exercise training," says the researcher. The evidence was clear. There was significantly less PGE2 in blood samples taken at the end of the programme than in samples taken before the training.
MHH study on SARS-CoV-2: Cross-vaccination protects effectively

Combination of vaccines from AstraZeneca and Biontech/Pfizer protects particularly well - even with virus variants.
Stand: 15. July 2021
The Standing Committee on Vaccination (STIKO) supports a second vaccination with an mRNA vaccine such as the one from Biontech/Pfizer for people under 60 who have already received an AstraZeneca vaccination – based on risk-benefit considerations. This recommendation is based on various research papers that were in preliminary stages of publication in scientific journals. Now the results of a study at the Hannover Medical School (MHH) by Professor Dr Reinhold Förster, head of the Institute of Immunology, and Professor Dr Georg Behrens, Clinic for Rheumatology and Immunology, were published in the journal Nature Medicine. The study has now shown that such a cross-vaccination is more effective against SARS-CoV-2 infections than the double vaccination with the AstraZeneca vaccine. In addition, it is more effective against virus variants. The study was supported within the framework of the German Center for Infection Research (DZIF) and financially supported by the Cluster of Excellence RESIST, the State of Lower Saxony, the Federal Ministry of Education and Research (BMBF) and Collaborative Research Centre 900.
The researchers compared the immune responses in blood samples from 175 volunteer study participants, one-third of whom chose AstraZeneca for their first vaccination and two-thirds of whom chose Biontech/Pfizer for their second vaccination. The study participants were MHH employees.
Cross-vaccination: Strong immune response and more protection against virus variants
"The second vaccinations with the Biontech/Pfizer vaccine led to significantly stronger immune responses than the second vaccinations with the AstraZeneca vaccine," reports Professor Förster: "After the cross-vaccination, there was an 11.5-fold increase in certain protective antibodies (anti-S IgG), whereas the AstraZeneca vaccination alone led to about a three-fold increase. There were similar changes in other antibodies (anti-S-IgA) and in T cells. The quality of antibodies and T cells was also higher after cross-vaccination. Antibodies keep the virus from entering the cells. T cells destroy infected cells and trigger further immune reactions. "The overall effect of the cross-vaccination was similar to that of people fully vaccinated with the Biontech/Pfizer vaccine," says Professor Behrens. However, he adds, the immune response is already at a very high level even with AstraZeneca vaccination alone, and the vaccine remains very important in the fight against COVID-19.
Another key advantage of cross-vaccination is that - according to the values determined by the researchers in the laboratory - it also protects more strongly against the alpha, beta and gamma virus variants. In contrast, the immune response to these variants often remained weak after the double AstraZeneca vaccination. "We are now testing the immune response to the virus variant delta, whose share of new infections in Germany is currently a good six percent," says Professor Förster. "A double vaccination with the Biontech/Pfizer vaccine also protects very well against infections with the four virus variants addressed, this is known from other studies."
Good basis for recommendations on vaccination sequence
"We already have to think about what the immunity situation will be in late summer and autumn, and based on this situation we have to decide which groups need a third vaccination and with which vaccine they should be vaccinated," says Professor Förster. "Our study, together with other work from other research institutes, forms a good basis for recommendations of the vaccination sequence. A different vaccine could be used specifically for a booster vaccination - also, for example, to be able to react to new mutations that could emerge at any time," adds Professor Behrens.
RESIST - Research for the Weakest
Professor Förster is co-spokesperson of the MHH-led Cluster of Excellence RESIST (Resolving Infection Susceptibility), in which around 50 research teams are working towards one goal: They want to better protect particularly susceptible people from infections. RESIST includes physicians working in the clinic who are very familiar with the situation of patients, as well as basic scientists who research pathogens and their interaction with the immune system down to the smallest detail. RESIST consists of six partner institutions, the spokesperson is Professor Dr. Thomas Schulz, head of the MHH Institute of Virology. RESIST is funded by the German Research Foundation (DFG). More information about RESIST can be found at www.RESIST-cluster.de .
In the German Center for Infection Research (DZIF), around 500 scientists and doctors from 35 institutions – including the MHH – are working together to develop new approaches to the prevention, diagnosis and treatment of infectious diseases. The goal is so-called translation: the rapid, effective implementation of research results in clinical practice. In this way, the DZIF paves the way for the development of new vaccines, diagnostics and drugs against infections. Further information can be found at www.dzif.de.
MHH project "COVID-19 cohort" helps clarify disease risk
International research network discovers genetic markers for severe COVID-19 progression

Stand: 09. July 2021
What factors are responsible for the fact that some people become severely ill after infection with the SARS-CoV-2 coronavirus, while others develop only mild symptoms or none at all? This question is being investigated by scientists in an international consortium called the COVID-19 Host Genomics Initiative. In addition to smoking and obesity as risk factors for a severe COVID-19 course, the research team has also found genetic factors in the human genome that apparently play an important role. Hannover Medical School (MHH) is also involved in the worldwide collaboration. It has contributed biosamples and data from its "COVID-19 cohort", a research project supported by the Lower Saxony Ministry of Science and Culture (MWK) with more than two million euros. The first results from the studies of the worldwide research network have now been published in the scientific journal Nature.
Data from Hannover for worldwide study
Biosamples and data from the "COVID-19 cohort", which have been collected and compared since March 2020 from patients with varying degrees of SARS-CoV-2 coronavirus and control samples from people with other respiratory diseases from various MHH clinics and the Klinikum Region Hannover, come from the MHH. The COVID-19 biobank is housed in the Hannover Unified Biobank (HUB). "The HUB meets the high security requirements for processing and storing the biosamples," emphasises Professor Dr. Thomas Illig, head of the HUB. For its analysis, the "COVID-19 Host Genomics Initiative" has brought together clinical and genetic data from almost 50,000 patients worldwide who tested positive for the virus, as well as from two million control subjects from numerous biobanks and clinical studies.
Genetic starting points for new therapy strategies
"When analysing the genetic data, 13 sites were found in the human genome that are strongly associated with infection or severe COVID-19 courses," explains Professor Dr. Markus Cornberg, Deputy Director of the MHH Clinic for Gastroenterology, Hepatology and Endocrinology and Director of the Centre for Individualised Infection Medicine (CiiM), who is responsible for the clinical processing of the samples stored at the HUB. Some of these gene loci also appear to be linked to autoimmune diseases, lung cancer or pulmonary fibrosis, a pathological proliferation of connective tissue, which then hardens and scars (fibroses) and leads to shortness of breath. "These results could help to find targets for future therapies," says the infectiologist. And that is urgently needed. While vaccines offer protection against SARS-CoV-2 infection, there is still considerable room for improvement in COVID-19 treatment.
The "COVID-19 Host Genomics Initiative" is one of the most extensive collaborations in human genetics and currently includes more than 3.500 authors of 61 studies from 25 countries. In addition to the Hannover Unified Biobank (HUB) and the MHH Clinics for Gastroenterology, Hepatology and Endocrinology, for Pneumology, for Renal and High Pressure Diseases, for Rheumatology and Immunology as well as the COVID Outpatient Clinic, the Hannover Region Hospital, the Centre for Individualised Infection Medicine (CiiM) and the Helmholtz Centre for Infection Research are also involved in the Hannover project "COVID-19 Cohort".
The original paper "The COVID-19 Host Genetics Initiative. Mapping the human genetic architecture of COVID-19" can be found here.
How useful are COVID vaccinations for children?

Stand: 02. July 2021
For a few weeks now, young people between the ages of 12 and 17 can get vaccinated against COVID-19. The European Commission has approved the vaccine from Biontech/Pfizer for this age group. However, the Standing Commission on Vaccination (STIKO) at the Robert Koch Institute (RKI) does not want to generally recommend vaccinating children and adolescents because the data basis is still too thin. We asked Dr. Nikolaus Schwerk, senior physician in paediatric pneumology, allergology and lung transplantation, about this.
Dr Schwerk, do you share the current reluctance of the Standing Commission on Vaccination to vaccinate children against COVID?
Answer: This question cannot be answered in one sentence. First of all, one must bear in mind the goal of a nationwide vaccination recommendation for children in Germany, which is issued by the STIKO. The aim is to prevent and, in the best case, eradicate infections that lead to serious illness or even death in a relevant proportion of children. In addition, the vaccines must be safe, i.e. the ratio of benefits and risks must be carefully weighed. The STIKO has an extremely responsible task here.
Fortunately, only very few children become seriously ill in the case of an infection with SARS-CoV-2 and most of them even show asymptomatic courses. In Germany, there are currently about 13.5 million children between the ages of 0 and 17. Since the outbreak of the pandemic, 367,914 infections and 14 deaths due to or in connection with a SARS-CoV-2 infection in children aged 0 to 14 years have been reported to the RKI (as of 29.06.2021). It should be noted that many infections in this age group were certainly not recognised or reported in the first place, so we must assume a much higher number of unreported cases. The extremely low number of severe courses of the disease also corresponds to my personal experience in our clinic, where so far no child has died of a SARS-CoV-2 infection and fewer than ten patients have had to be treated as inpatients in the entire period, mostly only with mild symptoms. So you would have to vaccinate an extremely large number of children to prevent severe or even fatal SARS-CoV-2 infections. Therefore, I can well understand the STIKO's reluctance.
However, it must also be admitted that the risk groups for children named by the RKI and the STIKO are somewhat arbitrary. It is true that children with a wide variety of chronic or severe previous illnesses were overrepresented in percentage terms in the case series of severe courses of illness caused by SARS-CoV-2 published to date. However, this is not surprising, since children with a severe and/or chronic illness generally have an increased risk of severe infectious diseases. This was already the case before COVID-19. However, the risk depends on the specific underlying disease of the child, the current state of health, the ongoing therapy and also the age. Therefore, due to the extremely low numbers of severe disease courses, specific risk groups could not be clearly identified to the best of my knowledge.
Do you have any concerns about possible side effects of the vaccine?
Answer: I believe that the available vaccines are safe and, due to their mechanism of action, I cannot imagine that late effects are to be feared. I cannot prove this, but can only give my own personal assessment here.
In your opinion, are there any aspects that speak in favour of vaccination?
Answer: In my opinion, the question of whether or not children should be vaccinated against SARS-CoV-2 must also take into account the negative socio-psychological effects of this pandemic. In my opinion, these are dramatic and their extent cannot yet be clearly estimated. We should also not tell ourselves that the pandemic is over. A fourth wave is also quite possible in Germany. In this case, the vaccination could be very useful for the children, as it would possibly enable them to continue going to school, meeting friends or playing sports in a club even if the number of infections increases. I think these arguments are very relevant and should be included in the decision for or against vaccination.
How do you deal with this question with your own children?
My wife and I did it with our children (12 and 15 years old) as follows: We talked to them and gave them the option of being vaccinated if it is ensured that all those who are really at risk and willing to be vaccinated have received their vaccination. Unfortunately, this is still far from being the case. Both children immediately decided to get vaccinated, even though they hate injections. And my wife and I have no worries at all about possible relevant undesirable side effects.
The Delta variant is considered to be much more contagious, especially among young people. What advice do you give to parents who are unsure whether they should have their child vaccinated?
Answer: Basically, with regard to the delta variant, the same protective measures should be adhered to as before.
The questions were asked by: Vanessa Meyer
Lessons from Corona: More closeness at the end of life

MHH investigates effects of the Corona pandemic on outpatient palliative care in PallPan.
Stand: 23. Juni 2021
The Palliative Care in Times of Pandemic (PallPan) research network has presented the "National strategy for the care of seriously ill and dying people and their relatives in times of the pandemic". At the heart of the strategy are specific recommendations for action on how to enable closeness at the end of life in particular in the event of future pandemics. Hannover Medical School (MHH) is also involved in the research project: A team from the Institute of General Medicine and Palliative Medicine led by Professor Dr Stephanie Stiel and Institute Director Professor Dr Nils Schneider has examined aspects of general outpatient palliative care.
16 studies with more than 1,700 people affected by palliative care
The PallPan research network of the National Research Network of University Medicine on Covid-19, Network University Medicine (NUM) consists of palliative medicine facilities of 13 university hospitals and is dedicated to the experiences, burdens and challenges in the care of seriously ill and dying people in the current pandemic. In 16 studies over a period of nine months, more than 1,700 patients, caregivers and responsible persons in the health system and in politics were asked about their experiences and their statements were systematically examined and evaluated.
The MHH team focused on the survey of general practitioners and oncologists in private practice. "In the first phase of the pandemic, the focus was mostly on COVID-19 sufferers in inpatient care," says Professor Stiel. "People with other diseases, on the other hand, have been lost from view." For oncologists in private practice, there were initially problems with adapting practice procedures to the hygiene regulations caused by the pandemic. Making appointments for chemo and transfusion therapies was also more difficult in the initial phase because patients were still uncertain at first. However, that quickly subsided. "The oncologists interviewed also reported that there were hardly any losses in the quality of treatment," emphasises Professor Stiel.
"Care and end-of-life care for the seriously ill has deteriorated"
However, GPs had to deal with other difficulties besides the reorganisation of their practice procedures. They were able to make fewer visits to patients at home and in care facilities due to the pandemic-related contact restrictions and visiting bans. "From a GP perspective, this has led to a deterioration in the care of seriously ill and dying people," Professor Schneider emphasises. This not only has an impact on physical health. The mental state of the sick and their relatives has also suffered. "General restrictions on contact and bans on visits to care facilities have not done people at the end of life and their relatives any good," Professor Schneider emphasises. GPs therefore wished to be involved in local crisis teams so that the concerns of people at the end of life and their relatives would be adequately taken into account in the future.
33 recommendations for action
With the help of 120 experts from the various areas of health care, administration and politics, the results of the 16 studies from the 13 university hospitals were developed into a common strategy and coordinated. The core of the strategy are 33 concrete recommendations for action, which are divided into three sections: Supporting patients and their relatives, supporting staff and supporting and maintaining palliative care structures and services.
According to the results of the survey, patients and their relatives want one thing above all for the future: to enable closeness at the end of life even in a pandemic. This requires balanced visiting regulations for institutions such as hospitals and care facilities, but also a legal framework, which politics must create. Case-by-case decisions and clearly defined exemptions have proven to be a workable and helpful strategy and should be used everywhere. Healthcare workers need above all sufficient protection against infections, but also basic palliative care knowledge and psychosocial support in challenging situations, for example in intensive care units or nursing homes. "Even in times of a pandemic, seriously ill and dying people are entitled to good symptom treatment and dignified care in accordance with the patient's will. This applies to both infected and non-infected people. In the increased stress of a pandemic, those providing care need more support," emphasises Professor Dr. Steffen Simon from the University Hospital of Cologne and one of the two coordinators of the PallPan network.
On the part of politics as well as clinics and care facilities, attention must be paid to ensuring that palliative care structures are maintained even and especially in a pandemic situation. "Palliative care units must not be closed in a pandemic; rather, outpatient and inpatient palliative care services should remain operational for the necessary care of seriously ill and dying patients and, if necessary, be adapted or even expanded - for example, for infected patients who can not be cured," appeals Professor Dr Claudia Bausewein from LMU Klinikum München, also coordinator of the PallPan network and President of the German Society for Palliative Medicine (DGP).
Information platform and bereavement services
The PallPan network is already planning further projects: the establishment of a web-based information platform, the development of support materials for bereaved relatives and staff in care facilities and hospitals, the integration of PallPan into a "National Pandemic Preparedness" for the German health care system and the continuous further development of the recommendations for action.
The PallPan research association is funded by the BMBF as part of the Network University Medicine (NUM). The research association includes the palliative medicine facilities of the university hospitals in Aachen, Bonn, Düsseldorf, Erlangen, Freiburg, Göttingen, Hamburg, Hanover, Jena, Cologne, Munich, Rostock and Würzburg. Professor Claudia Bausewein from the LMU Hospital in Munich and Professor Steffen Simon from the University Hospital in Cologne are the overall coordinators.
SERVICE:
Link to PDF: https://doi.org/10.5281/zenodo.5012504
The PallPan Consortium invites you to a virtual final conference where the National Strategy will be presented. (pall.pandemie@med.uni-muenchen.de) The date is 24 June 2021, from 2 pm to 5.30 pm. Participation is free of charge, registration is not necessary. Dial-in link (identification code: 562238): https://lmu-munich.zoom.us/j/95257337713?pwd=TW5Ib1BnYmNVWFBEMUEvTksrTk95QT09
Keyword
Providing optimal care for patients, preventing infections, preserving health care: The Covid-19 pandemic brings with its challenges that require new strategies for action within a short period of time. The National Research Network of University Medicine on Covid-19, in short Network University Medicine (NUM), bundles and strengthens research activities to cope with the current situation. Funded by the Federal Ministry of Education and Research and coordinated by the Charité - Universitätsmedizin Berlin, the research network involves all German university hospitals and other networks in working on solutions for the best possible patient care during the pandemic. 13 comprehensive collaborative projects with leaders at the various university medicine sites have been designed for this purpose. The programme is designed to provide rapid, immediate support. Emphasis is placed on clinic-related research and health care research, the results of which flow directly into health care and crisis management in accordance with the translational approach. The research network and the participating institutions have around 150 million euros available in the first year to implement this task; from 2021, the network is to be funded with a further 80 million euros annually until 2024, or an additional 240 million euros. Joint developments in research and patient care, evidence-based approaches and mutual learning should lead to a common approach to pandemic control and "pandemic preparedness". Further information: www.netzwerk-universitaetsmedizin.de
MHH: Young woman successfully lung transplanted after COVID-19 infection

Status: 27. Mai 2021
Hannover Medical School (MHH) has transplanted a lung into a patient severely affected by COVID-19. For the 34-year-old, it was the only therapy still possible. After careful evaluation, an interdisciplinary team at MHH decided on the transplant in early May 2021. The patient, who was pregnant at the time of the infection, as well as her child are now doing well. "The case illustrates MHH's expertise in the care of patients severely affected by COVID-19 at all stages of the disease," Professor Dr. Frank Lammert, Executive Board member for Health Care, points out.
Child delivered by cesarean section
In early March 2021, the pregnant patient had been admitted to MHH with a COVID-19 infection. Her stable condition deteriorated visibly over the course of a week: after an initially successful week of non-invasive mask ventilation (NIV), she had to be intubated and artificially ventilated due to advancing lung failure. Immediately after intubation, the intensive care physicians, together with Professor Dr. Constantin von Kaisenberg, Division Head of Prenatal Medicine and Obstetrics at the MHH Department of Obstetrics and Gynecology, and the neonatologists at the Children's Hospital, decided to perform a cesarean section at the 34th week of pregnancy because they expected the mother's health to deteriorate further. There was already a very good chance of survival for the child outside the uterus. In addition, the doctors expected that the patient would be easier to ventilate after cesarean section and that treatment with an artificial lung, extracorporeal membrane oxygenation (ECMO), would be more promising.
Infection irreversibly damaged the lung
The decision turned out to be correct only a few days later. The condition deteriorated so rapidly that an artificial lung (ECMO) became necessary to provide the patient with sufficient oxygen. Due to massive and irreversible damage to the lungs, the intensive care physicians, together with the pulmonologists who were called in, finally examined whether a lung transplant could be considered as the ultima ratio. "The patient's lungs were very badly damaged by the infection. There was no longer any prospect of the lungs recovering despite all intensive medical measures," says Professor Marius Höper, M.D., vice director of the Department of Pneumology. "That's why, after careful evaluation, we ultimately decided on a transplant together with the intensive care physicians and surgeons."
Artificially ventilated with ECMO for 40 days
To evaluate the patient for transplant, she had to be responsive. "Often patients are sedated when they are artificially ventilated," explains Professor Wolfgang Koppert, M.D., director of the Department of Anesthesiology and Intensive Care Medicine. "In a total of nine weeks, the doctors, nurses and physiotherapists on Ward 44 worked hard to ensure that the patient could be awake and thus responsive during artificial ventilation." In total, the patient was dependent on artificial lungs (ECMO) for more than 40 days.
In addition to irreversible damage to the organ, other criteria had to be met before a transplant could be performed: she could not have any relevant previous diseases that could have threatened the success of the transplant, and she could no longer have an acute COVID-19 infection. "Our criteria for listing the patient were that she had no neurological deficits, no damage to other organs, and could comply with the lifelong therapy associated with the transplant," says Professor Axel Haverich, MHH Director of Cardiothoracic, Transplantation and Vascular Surgery and Head of the MHH Transplant Center, "The patient met all of these."
Interdisciplinary expertise at MHH
The patient's care involved physicians, nurses, physical therapists and perfusionists from numerous disciplines - from intensive care physicians and pulmonologists to the women's and children's clinics, surgeons and anesthesiologists. "The situation was completely different from what usually happens in lung transplantation, where patients are usually evaluated over a period of six months and are able to deal with the situation mentally during this process," explains Professor Höper.
Mother and child are now doing well
For patients whose lungs are irreversibly damaged after COVID-19 infection, transplantation may be the last therapeutic option. To date, about 40 of these patients have received lung transplants worldwide. Three additional cases are known throughout Germany. "In the COVID-19 transplants performed so far, it was reported that the damage to the lungs had made the operation more difficult. However, this was not the case with our patient," explains Professor Dr. Haverich. "The surgery proceeded without further complications. The patient also did not need to be artificially ventilated with ECMO again after the operation," says the surgeon. "After only a few days, breathing started spontaneously." Two weeks after transplantation, she was able to leave the intensive care unit. The transplanted lungs are fully functional. "There is a good chance for a full recovery." Mother and child are now doing well.
New visiting regulations for relatives!
As of Monday, 17 May, visits by relatives are possible again under certain conditions.

Status: 14. May 2021
The general ban on visits by relatives at Hannover Medical School (MHH), which has been in place since 26 March, has been lifted. From Monday, 17 May 2021, the following new visiting regulations will apply:
- One visitor per day for one hour in the time from 2 p.m. to 6 p.m. is possible.
- Visits must either be pre-registered online (see here) or at the service points
- Fully vaccinated visitors do not need a test certificate, but must show their vaccination card.
- Those who have not been fully vaccinated require an up-to-date test (antigen or PCR test) with official certification from an accredited testing centre
The MHH does not offer testing facilities!
In the delivery room, in the paediatric clinic and for relatives of patients receiving palliative care, the previously existing visiting rules continue to apply.
Further information is available at https://corona.mhh.de/visit.
New findings on rare side effects after Corona vaccination
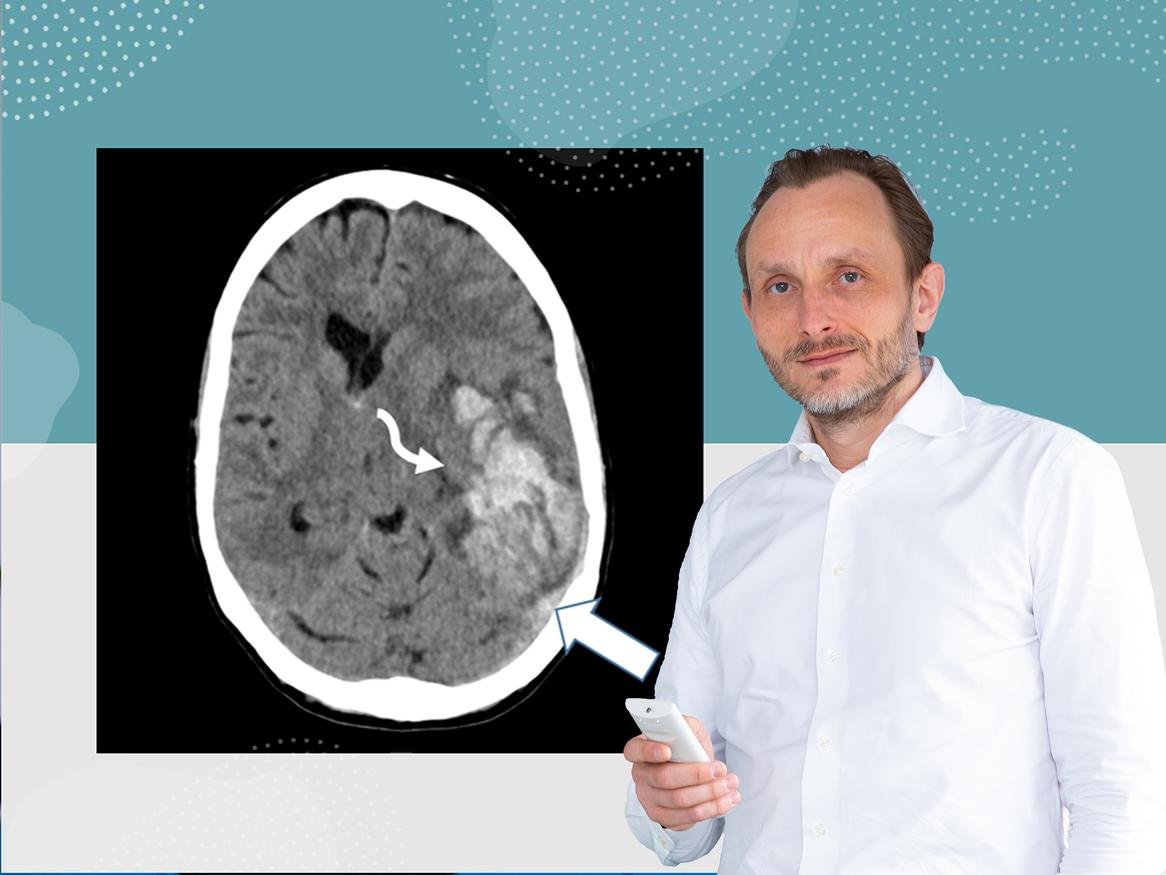
MHH successfully treats patients with sinus vein thrombosis.
Status: 03 Mai 2021
Since mid-March 2021, rare cases of cerebral venous thrombosis (sinus vein thrombosis) have occurred in Germany and other countries after vaccination against the SARS-CoV-2 coronavirus with AstraZeneca's vaccine (Vaxzevria). The side effect of the vaccination can result in a decrease in the number of platelets (thrombocytes) in the blood of those affected and is therefore also called vaccine-induced thrombotic thrombocytopenia (VITT). Five patients referred from various clinics in Lower Saxony and North Rhine-Westphalia were treated at the Hannover Medical School (MHH). As the first German clinic, the MHH has now evaluated its detailed experience in diagnostics, disease progression and therapy and made it available to the international medical community as a treatment recommendation. The results have been published in the renowned journal Blood. The first author is Dr. Andreas Tiede, Professor of Haemostaseology at the Department of Haematology, Haemostaseology, Oncology and Stem Cell Transplantation.
Vascular occlusions in veins and arteries
The cause of this rare side effect is a misdirected reaction of the immune system. This leads to the formation of antibodies against a protein of the blood platelets that is produced naturally in the body, platelet factor 4 (PF4). "We have detected PF4 antibodies in all affected patients with VITT," says clinic director Professor Dr Arnold Ganser. If the antibodies bind to PF4, the platelets can be activated, as would be the case if a wound were healing. If there is no bleeding, clots can form in the blood - thrombosis. In addition, the doctors who treated the patients noticed an overall decrease in blood platelets (thrombocytopenia), as well as vascular occlusions. However, these thromboses did not only affect the brain veins, but also the veins of the abdominal organs and the arteries in the brain and legs. The patients had to be treated differently depending on the severity of the disease - with blood thinners to prevent the spread of thrombosis, but also with cortisone and other drugs. The therapy was successful for all of them, and three have since returned home. "For the patients, it was life-saving that, on the one hand, we have enough highly specialised intensive care beds and, on the other hand, we are a maximum care hospital where specialists from the most diverse disciplines work together 24 hours a day, 7 days a week," emphasises MHH President Professor Dr. Michael Manns. Only the interdisciplinary cooperation of colleagues from different medical departments has made it possible to detect and effectively treat a new type of disease within a few days.
Quick action for signs of thrombosis
"Fortunately, the complication VITT is very rare," says Professor Tiede. Early diagnosis and treatment are crucial for a cure, he says. However, headaches and mild fever one to two days after vaccination are normal signs of an immune reaction and no reason to worry. However, anyone who still has severe symptoms after more than four days should see their family doctor immediately. A blood count taken there will provide information about possible signs of VITT. "In this case, the patient must immediately go to the emergency room of a hospital," advises the physician. The publication that has now been published, in turn, gives the treating clinics precise indications as to which treatment is then sensible.
The publication is the result of interdisciplinary cooperation between several MHH clinics and institutes. In addition to the Department of Haematology, Haemostaseology, Oncology and Stem Cell Transplantation, this also includes the Institute of Clinical Chemistry, the Department of Neurosurgery, the Institute of Neuroradiology, the Department of Neurology with Clinical Neurophysiology and the Department of Gastroenterology, Hepatology and Endocrinology.
The original paper "Prothrombotic immune thrombocytopenia after COVID-19 vaccine" can be found here.
MHH commemorates the Corona dead

German Federal President Frank Walter Steinmeier has announced a memorial service for people who died as a result of a Corona infection on 18 April, we too will be taking part.
16 March 2021
Uwe Keller-Denecke, pastor of the Protestant Pastoral Care at the MHH, explains what it's all about:
Why are we doing this?
The central commemoration in Berlin on 18 April is an important signal from the Federal President to civil society. We are taking this on board locally and want to support and strengthen it. People at the MHH have also died from and with COVID-19. We commemorate them with this minute's silence. Our sincere sympathy goes out to their families and loved ones!
The minute's silence is also an expression of our solidarity with all those in nursing and medicine who have stood by the sick. They were able to help many back to life and also had to accompany some to their death. This cost a lot of energy and sometimes took us to our limits.
For this, the staff deserves our greatest thanks and deepest respect.
Who can join in?
Everyone in the various places of the MHH, in the corridors, in the rooms. In wards and doctors' rooms, indoors or outdoors in the patient garden or parking deck.
In the main building, the events in the chapel will be heard over the patient radios at the beds, and at 13.30 we would like to sound a gong in the shopping street. But it doesn't matter to hit exactly half past two.
All those who know about it and are committed to this commemoration can be there in their own moment, whether as individuals or as teams.
They can be there by stopping work for a minute, wherever possible. Do nothing for a minute, remain silent, turn your gaze inwards. Breathe in, breathe out, follow the rhythm of life and give it space. To then return to the other people and the common work, in connectedness.
From 26 March there will be a general ban on relatives visiting the MHH!

Regulation will initially apply for four weeks / Arrangement of a pick-up and drop-off service.
Status: 24 March 2021
From Friday, 26 March 2021, a general ban on relatives visiting the MHH will apply again due to the rising incidence figures and the current resolutions of the federal and state governments. The regulation is initially valid for four weeks. The delivery room and maternity ward as well as the paediatric clinic are exempt from this regulation. The existing rules continue to apply there, for further information see here. There is also an exception for relatives of patients receiving palliative care. The ban on visitors serves to protect the patients and the staff members of the clinics. Accompanying persons (if necessary) for outpatients are still allowed.
Arrangement of a pick-up and drop-off service
A pick-up and delivery service has been set up to ensure that inpatients' relatives can continue to provide them with the necessary items and laundry. Relatives can drop off the necessary items at the Service Point in the main hospital on weekdays between 2 pm and 7 pm.
First Europe-wide guideline for the inpatient treatment of COVID-19 patients

MHH pneumologist is co-author and representative for Germany
Status: 19 March 2021
With the onset of the Corona pandemic, the feverish search for vaccines and effective drugs against the SARS-CoV-2 virus also started. In research, activities are running at full speed. Hundreds of new scientific papers on the virus and the COVID-19 disease are published every day. Now, for the first time, the European Respiratory Society (ERS) has published a European guideline for the inpatient treatment of COVID-19 patients. Professor Dr. Tobias Welte, Director of the Department of Pneumology at the Hannover Medical School (MHH), is co-author and representative of the guideline in Germany.
Pragmatic instructions for action
The focus of the ERS guideline is on drug therapy in hospital. "The recommendations are very clear for all phases of inpatient therapy," explains Professor Welte. For example, it is not recommended to use the drug Remdesivir in hospitalised patients - according to the data in the guideline, it is not effective. Whether Remdesivir can play a role in a very early phase of the disease, in largely symptom-free patients in the outpatient setting, has not yet been conclusively clarified. In the late phase of COVID19, the immune system of those affected can trigger faulty, often excessive inflammatory processes. Cortisone is used against this; this is explicitly recommended in the guidelines. In very ill patients, however, the administration of antibodies against the messenger substance interleukin 6 is also recommended. Throughout the course of COVID-19, blood clots can form in the capillary system of the lungs. In this case, the recommendation is to use a blood thinner, such as Heparin, as usual.
"Whether additional anticoagulant agents, such as inhibitors of platelet aggregation like ASS, should be administered still needs to be clarified," explains Professor Welte. In addition to drug recommendations, the guidelines also contain recommendations on oxygen administration and ventilation for COVID-19 patients. The guideline is provided with commentary in between. The pneumologist sees this as a great advantage: "The pragmatic instructions for action are comprehensible for all those involved in the treatment."
Constant updating
The ERS guideline not only incorporates countless published scientific papers, but also studies that are only about to be published. The so-called GRADE system was used in the preparation of the guidelines. In this methodology, a quality assessment of the studies is made according to their evidence, and this quality in turn has an impact on the strength of a recommendation. Since new scientific knowledge about the virus and the disease is gained every day, the ERS guideline is also constantly updated. Professor Welte expects a new version in a few weeks. He hopes that the guideline will be implemented in as many clinics as possible.
Fortunately, the ERS recommendations now published for Europe do not differ significantly from the German guidelines recently published in the journal “Deutsches Ärzteblatt”.
The European Respiratory Society is the largest scientific and clinical organisation for pulmonary and bronchial medicine in Europe. The ERS guideline was published in the European Respiratory journal.
SARS-CoV-2: T-cell immunity plays important role in virus defence

Research group investigates immune response in blood samples of COVID-19 sufferers and recovered patients.
Status: 08 March 2021
How severely we actually contract COVID-19 after infection with SARS-Cov-2 depends on our immune system. Antibodies, which are supposed to prevent the viruses from entering the cell as a so-called humoral immune response, are decisively involved. The concentration of these protein compounds decreases over time - especially in patients who have only had a mild course of the disease. But our immune system knows another way to fight viruses: the cellular immune response with the help of T-lymphocytes. They belong to the white blood cells and seek out cells affected by the virus in order to destroy them and thus prevent further virus spread in the body. A research team led by Professor Dr. Rainer Blasczyk, Director of the Institute of Transfusion Medicine and Transplant Engineering at the Hannover Medical School (MHH), and Professor Dr. Britta Eiz-Vesper has investigated precisely this aspect of the virus defence and proved that T-cell immunity plays an important role in lasting protection against SARS-CoV-2. The study in cooperation with the University Hospital Essen has now been published in the renowned journal "Immunity". First author is Dr. Agnes Bonifacius.
Concentration of immune cells remains largely stable
"Until now, there was a lack of data on cellular immunity against SARS-CoV-2 during the disease and beyond," says Professor Blasczyk. The scientists therefore analysed blood samples from COVID-19-genese patients with those from acutely ill and healthy, non-infected (SARS-CoV-2-seronegative) control groups and compared both the antibody level and the concentration of T-lymphocytes. They found that those who had recovered did not have as many antibodies in their blood as those who were immediately ill. However, the scientists were able to detect a high number of memory T effector cells specialised in SARS-CoV-2. These not only recognise the crown-like spike protein, but also other structures of the virus surface. As immunological memory, they also improve protection in the event of renewed infection with the same pathogen. "Apparently, T-cell immunity remains unchanged after COVID-19, although the antibody concentration drops sharply," the transfusion physician notes.
"Apparently, T-cell immunity remains unchanged after COVID-19, although the antibody concentration drops sharply," the transfusion physician concludes.
Earlier contact with harmless coronaviruses protects
Contact with other members of the coronavirus family, which cause harmless flu infections, for example, apparently also has a favourable effect on the SARS-CoV-2 defence. "An existing immunity against such endemic coronaviruses has a positive effect on the development of T-cell immunity against SARS-CoV-2 and thus presumably also on the course of COVID-19," explains Professor Eiz-Vesper. This cross-immunity is particularly interesting with regard to virus mutations. "If it already helps against a more distantly related coronavirus, the effect could be much greater with the SARS-CoV-2 variants, which are much more similar to each other," the scientist suspects.
This question will now be clarified in a next study. In addition, the scientists want to investigate whether T cells could also be used therapeutically for certain moderately severely ill patients with COVID-19. -n. Similar to the treatment with the blood plasma of convalescents, in which the administration of antibodies against SARS-CoV-2 is supposed to prevent severe disease progression, donated T cells could also help against COVID-19. "In certain patients, we see a lack of their own T cells or observe that the defence cells are less active," explains the immunologist. The results could then not only help to better predict disease progression, but also lead to more successful vaccination strategies.
The study was conducted in cooperation with the University Hospital Essen, the German Centre for Infection Research (DZIF), the Centre for Individualised Infection Medicine (CiiM), the MHH Clinic for Gastroenterology, Hepatology and Endocrinology, the MHH Clinic for Pneumology, the MHH Clinic for Renal and Hypertension Diseases, the MHH Clinic for Paediatric Haematology and Oncology and the Hannover Public Health Department.
Coronavirus: How dangerous are the mutations?
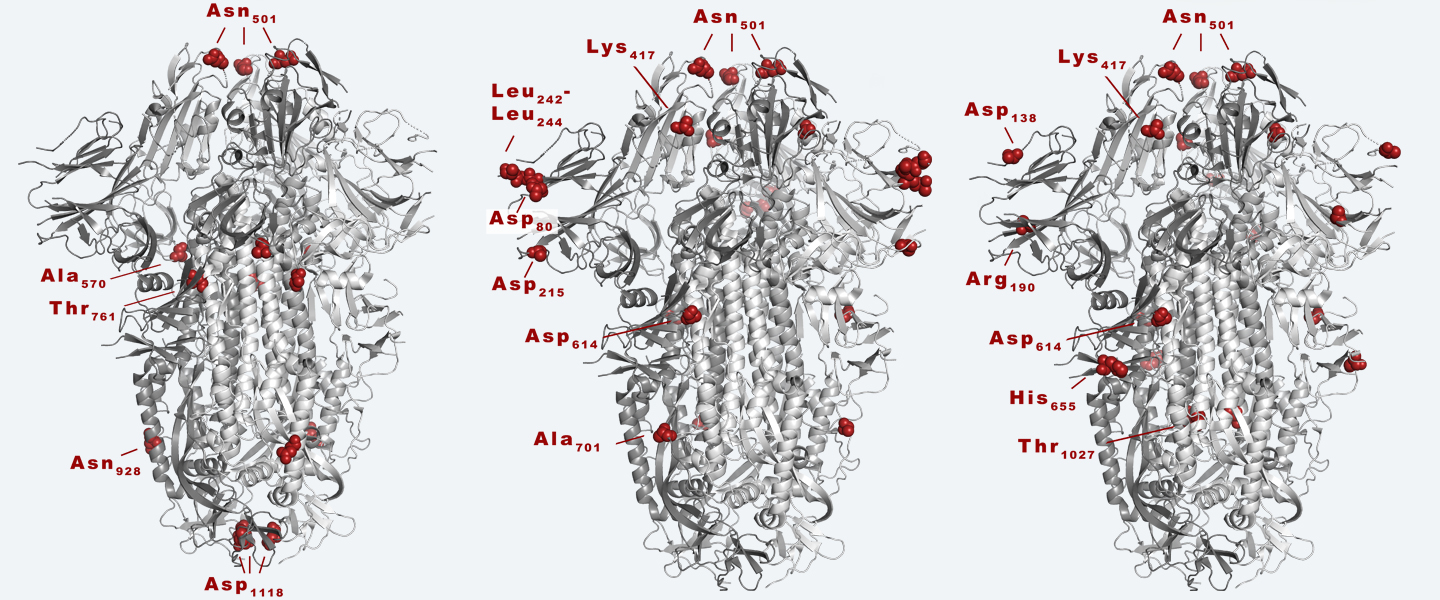
Mutations of the SARS-CoV-2 coronavirus are on everyone's mind these days. Professor Dr Thomas Schulz, head of the MHH Institute of Virology and Speaker of the Cluster of Excellence RESIST, answered our questions on this topic.
Status: 11 February 2021
Professor Schulz, there are British, South African and Brazilian variants of the SARS-CoV-2 coronavirus in Germany. How dangerous are these variants?
In the case of the English variant called B.1.1.7, it is relatively certain that it is more easily transmissible by about 30 to 50 percent, than the variants we have had in Germany so far. This means that, on average, anyone infected with the new variant will infect more people than someone infected with the 'conventional' virus. This increases the risk of a rapid spread of the B.1.1.7 variant.
This variant was first discovered in the UK. But its exact origin is unclear; it was detected there due to good surveillance. It has caused massive problems in Ireland, for example, after infection levels there were rather low in early December 2020. It is also widespread in Portugal. In Denmark and Switzerland, this virus variant is currently spreading at a low level.
The B.1.1.7 variant is not only more contagious than the 'classic' virus, there is also initial data to indicate that it could be more pathogenic, meaning that more people die on average after infection. However, this needs further investigation.
The speed at which the South African variant called B.1.351 is spreading in South Africa indicates that it is also more easily transmissible. At the moment it is the dominant variant over there, but has been detected occasionally in other countries. For example, cases of infection with variant B.1.351 have been reported several times in recent days at various locations in the UK, without any apparent contact with South Africa. This indicates that variant B.1.351 may have already spread in the UK before having been detected; currently its distribution is still at a low level. Given the rapid potential for spread, this is a cause for concern.
In Brazil, several new virus variants are circulating. The variant known as "Brazilian variant B.1.1.248" first emerged in Japan among travellers returning from Brazil. So far, there is little data on this variant.
How often do these variants occur in Germany so far?
So far, the variants are all relatively rare in Germany. The B.1.1.7 (UK) variant accounts for about 6% of all infections in Germany at the moment, with most likely considerable regional variation. There have for example been a few outbreaks of the English variant in Hanover, but the public health department was able to control them. There have also been 'outbreaks of infection' in other cities, for example in Berlin, which could be traced back to the B.1.1.7 variant. Also, the South African variant has caused infections, just as the Brazilian variant has already been detected in Germany. In order to find out more precisely how widespread the new variants are in Germany, between five and ten percent of the reported new infections samples are now being sequenced. This serves the purpose of gaining a better overview of the spread of these and other mutants that may occur in the future. It is important to keep in mind that the more space you give the virus to multiply – that is, the higher the infection numbers in a population – the faster the virus can mutate and the more variants emerge. The appearance of the three new variants mentioned above in countries where infection rates are or were very high is a striking illustration of this. Furthermore, the appearance of these variants also proves that the vaccination campaign that is now starting is not only about protecting the population in 'rich' countries, but that it must be in our own interest in Germany that vaccination is carried out as quickly as possible in poorer countries. Only when everyone is safe are we safe!
Are the vaccines also effective against these virus variants?
Several variants can escape part of the antibody response that our bodies have built up after a vaccination or after surviving an infection. There is a possibility that this could become a problem regarding vaccinations. Early indications are that recently developed new vaccines, for example, do not protect as well against the B.1.351 as they do against 'classic' variants. However, according to current knowledge, the new vaccines should still provide at least partial protection against the variants mentioned and prevent severe disease. Perhaps an additional booster vaccination will become necessary for the variants mentioned. We must also be prepared to modify vaccines if necessary. We will be able to assess this better as soon as we have more experience with the vaccines that have already been approved and will be approved in the next few months. In general, we can assume that vaccines that provide a high level of protection will have fewer problems with the new variants than those that already provide only partial protection against the classic virus variants. Nevertheless, at present, a vaccine that provides partial protection is better than no vaccine!
To counter the spread of the virus, scientists have proposed maintaining the lockdown throughout Europe until the incidence falls below 10? What do you think of this "NoCovid strategy"?
I can see that this would be desirable from a virological point of view. Obviously, given the problematic new variants, the lower the incidence figures, the safer we are. So there is no doubt that we still have to significantly reduce the currently still high infection rates in Germany. However, in my opinion it will be difficult to gain sufficient acceptance for the measures required for the 'No Covid' goal. To achieve this goal, one would have to close the borders within Europe and – at the current incidence – sustain a hard lockdown for several months. Given the other problems involved (economy, schools, psychological side effects) I don't think this is realistic. If – hopefully – the number of COVID-19 deaths and severe illnesses will decrease in the coming months thanks to vaccination of those at particular risk (nursing home residents, the elderly, people with pre-existing conditions, those working in the health care system, etc.), the challenge for politicians will be to communicate that certain restrictions on public life cannot be lifted as quickly as we all would like. Achieving public acceptance for this should be the urgent goal.
The questions were asked by Bettina Bandel
Coronavirus: How at risk are children?

The transmission of the SARS-CoV-2 coronavirus in children has been discussed again and again for a year. Our experts, Prof. Dr. Peter Hillemanns (Director of the MHH Women's Clinic) and Dr. Nikolaus Schwerk (Paediatrician in the MHH Clinic for Paediatric Pneumology) clarify the current status.
Status: 9 February 2021
What symptoms do children show with Corona?
Children are infected in the same way as adults, but a high percentage of them are asymptomatic and very rarely become seriously ill. Typical symptoms include a cold, sore throat, cough, fever, diarrhoea and abdominal pain, as well as shortness of breath, hypoxaemia and pneumonia in the very rare severe courses. The number of infant deaths associated with SARS-CoV-2 infection remains extremely low.
Can the child become infected in the womb?
So far, we know that in only eight percent of the cases where pregnant women were infected with SARS-CoV-2 viruses, these viruses could be detected in the newborns. So the infection can be transmitted, but apparently only very rarely. Probably more significant is the fact that the antibodies of the infected mother are transmitted to the child via the placenta. We know this phenomenon of so-called nest protection from many other viral diseases such as measles. The transmission of antibodies protects the children very well. Whether this is also the case with COVID-19 is still open. This is currently the subject of much discussion.
What is the risk for newborns, for example during breastfeeding, if the mother is infected?
The greatest risk is direct transmission through close contact and droplet infection. So far, there is no evidence of coronavirus in breast milk. On the contrary, it has been proven that antibodies are also transmitted via breast milk. This means that the risk of infection during breastfeeding is negligible. Here, the advantages for the protection of the child clearly outweigh the disadvantages.
Which children have an increased risk of a severe course of the disease?
There are so few severe courses of the disease that no clear risk groups can be determined statistically. In principle, children with a severe underlying disease generally have an increased risk of severe respiratory infections. However, SARS-CoV-2 has not led to a noticeable or measurable increase in mortality (compared to previous years) in children with chronic diseases.
What role do children play in the spread of coronavirus?
If they are infected, they are also infectious. Whether they are less, equally, or more contagious than adults cannot be said. There are different opinions and study results on this. It depends on many factors. For example, when you cough a lot, you produce a lot of aerosol, which makes it easier to infect others. Since children are often asymptomatic, i.e. they do not cough more, this could theoretically mean that they are less contagious. But that is a hypothesis and there are many of them, in one direction and in the other. Conclusion: Infected children are potentially contagious and should therefore be isolated in the same way as adults in the event of a confirmed SARS-CoV-2 infection.
What long-term consequences can Covid 19 disease have in children?
Since we have only known about the virus for a year, we can't really say anything about long-term effects. I am not aware of any studies that have described indications of, for example, chronic fatigue syndrome in children after Covid-19. Since hardly any children develop severe lung diseases, nothing is known about chronic diffuse lung diseases in children after SARS-Cov-2 infection.
There are increasing reports of children developing the so-called Kawasaki syndrome - a severe overreaction of the immune system with fever and inflammation of the blood vessels, which in the worst case is fatal. There is a suspicion that COVID-19 can also be a cause. What do you know about this?
What is observed is not the increased occurrence of Kawasaki syndrome, but an independent inflammatory disease that has Kawasaki-like symptoms - the so-called PIMS (Pediatric Inflammatory Multisystemic Syndrome). There are many indications that there is a connection to SARS-COV-2 - that is, an exaggerated immune reaction to the infection. However, it is very difficult to prove a clear causal relationship, but of course this does not rule it out.
The questions were asked by: Vanessa Meyer
Immunotherapy does not increase the risk of severe COVID-19 course

MHH study examines disease courses of more than 800 SARS-CoV-2-infected multiple sclerosis patients.
Status: 4 February 2021
The risk of developing a severe COVID-19 course after a SARS-CoV-2 infection is significantly increased for people with risk factors such as advanced age, severe obesity, diabetes, high blood pressure or heart failure. A challenge for the treating physicians, however, is also the handling of chronically ill neuroimmunological patients who are treated with drugs that suppress the immune system. Scientists from the Department of Neurology at the Hannover Medical School (MHH) have now investigated whether the risk of a severe course of the disease increases for patients with multiple sclerosis (MS) when infected with the coronavirus as a result of the immunomodulating therapy. The study, led by Professor Dr. Thomas Skripuletz in cooperation with the University Hospital Essen and the Charité Berlin, has been published in the Journal of Clinical Medicine. The first author is Dr Nora Möhn.
There is a lot of uncertainty among those who treat and those affected by the disease
"For fear of possibly harming their patients, some treating physicians have even refrained from immunotherapy since the beginning of the pandemic," explains Professor Skripuletz. Even MS patients themselves have suspended their treatment out of uncertainty and postponed appointments at the MHH infusion outpatient clinic, for example. The scientists wanted to change this situation. In order to create a therapy decision based on facts, the case reports of various medical publications published to date were combined in the review. "We evaluated data on 873 MS patients who tested positive for SARS-CoV-2 and compared the courses of the disease," says Dr Möhn. The scientists found that patients who continued to be treated with immunosuppressive drugs became less severely ill and died less frequently than those without treatment with MS therapeutics. "This finding fits with our observations from the clinic," emphasises the neurologist.
Drugs apparently do not negatively affect viral defence
The scientists see a possible explanation for this in the excessive immune reaction caused by SARS-COv-2, which is suspected of causing more damage than the virus itself. This undesired hyperactivity of the immune system might even be attenuated by the immunomodulating drugs. "In any case, the data indicate that the drugs do not have a decisive negative influence on the virus defence, whereas untreated and severely affected MS patients are particularly at risk," says Professor Skripuletz. Previously published studies on other neurological diseases have come to the same conclusion. "It is therefore advisable to treat chronic neuroimmunological patients as best as possible so that they are as fit as possible," emphasises the physician.
How does the pandemic influence our thoughts and feelings?

MHH research group wants to record the effects of the lockdown with second Germany-wide Corona survey.
Status: 29 January 2021
The Corona pandemic continues and with it the increasingly severe restrictions in professional and private life. Already at the beginning of the first wave of infection last year, researchers from the Centre for Mental Health at the Hannover Medical School (MHH) conducted one of the first and largest surveys on the effects of the crisis on the psyche. They were able to show that the occurrence of the Corona pandemic and the measures taken to contain it led to increased stress, anxiety, depressive symptoms, sleep problems, irritability, aggression and domestic violence. Now the web-based study is entering a second survey phase. In addition to psychological well-being, the scientists are now taking a closer look at the personal attitudes of people in Germany.
Dwindling acceptance expected
"We want to know how the citizens of this country feel and what moves them," says Professor Dr. Tillmann Krüger, head of the study. "We are also interested in recording people's individual backgrounds and positions with regard to the pandemic and the measures taken." This is one way to better understand the different reactions, he said. The scientists expect a continuing psychosocial burden and - depending on the individual situation - a dwindling acceptance of the orders that have drastically changed the everyday life of the citizens. In the first survey in April last year, 60 percent of the more than 3,500 participants said they could cope very well or well with the changed situation and the corresponding measures. Almost one third of the respondents, on the other hand, stated that they could handle the situation badly or very badly. Women showed significantly higher depression and anxiety scores than men.
As in the first survey, the current survey also includes different questions about the current state of health, experience and the respective life situation. The web-based systematic survey is anonymous and uses self-report scales. All citizens over the age of 18 are invited to participate in the survey at the following link: https://ww2.unipark.de/uc/mhh_covid2021.
Corona vaccination: Facts against Fake News
There are many false reports circulating in the media on the subject of corona vaccination. Our infectiologist Prof. Dr. Matthias Stoll clears up rumours and lies.
Status: 02 February 2021
Wrong!
The short time of development has no influence on the quality, since all standards have been met that other vaccines also fulfil. For this purpose, far-reaching official regulations were created worldwide in the run-up to the vaccine trials, which created the conditions for rapid approval without compromising safety...
In addition, a lot of money was also invested by the researchers and vaccine manufacturers so that the clinical trials could be carried out without delay. Normally, researchers have to complete phase one before they can start phase two. However, due to the high priority, phase two was allowed to start even though phase one had not yet been completed.
For the development of the Corona vaccine, significantly more people were tested than for other vaccines that had been tested and approved in previous years. In addition, unlike most previous vaccination trials, special arrangements were made to include as many age groups as possible equally and also to recruit as many people with concomitant diseases as possible.
Wrong!
BioNTech and Moderna use a new technology, the mRNA vaccine. This does not vaccinate a viral antigen - as is usually the case - but its genetic code, i.e. the blueprint for it, so to speak. Since the genetic code of human cells is a DNA blueprint instead of an RNA one, an RNA cannot get into the DNA code in the human cell nucleus. So, in a way, our genetic material has a natural protection against reprogramming by RNA and vaccines derived from it. For the same reason, the vector vaccines from AstraZeneca as well as the vaccine still in clinical trials from Janssen, which are based on RNA vector viruses, are harmless with regard to changes in the human genome: our body cells naturally lack the necessary enzymes to rewrite an m-RNA or an RNA into a DNA. However, much more than such a step would be necessary for genetic information from an RNA vaccine or virus to enter our genome.
Wrong!
It was assumed that there were similarities between a spike protein of the SARS-CoV-2 virus and the protein that is necessary to build up the placenta. The antibodies that are formed would thus also have targeted the placenta protein. However, this similarity of the proteins does not exist.
Not quite!
For sufficient vaccination protection, vaccination must be given twice. The second vaccination roughly doubles the proportion of vaccinated people with sufficient immune protection. The probability of contracting COVID-19 after the second vaccination is 95 and 94 percent lower than in non-vaccinated persons. Incidentally, among the more than 60 vaccine candidates currently in clinical trials worldwide, i.e. not yet approved, are vaccines that only need to be vaccinated once.
Wrong!
The risk of dangerous side effects is far below 1 per mille, more likely even below 0.1 per mille. This rate must be seen in relation to the death rate - worldwide and across all age groups - of more than 2 percent among Covid 19 sufferers.
Moreover, severe vaccine damage usually occurs very quickly - as a rule, long-term side effects show up after eight weeks at the latest. What happens in the body afterwards is often no longer directly related to the vaccine, as it has long since been broken down by the body. The triggered immune reactions have also all expired and the immune system - specifically trained for the coronavirus - only remains in a "beware" position.
SARS-CoV-2 attacks the heart

MHH research team detects biomarkers for cardiovascular stress in the blood of COVID-19 patients.
Status: 21 Januar 2021
Infections with the SARS-CoV-2 coronavirus are not only a burden on the lungs. The virus also massively affects the cardiovascular system. A research group of the Institute for Molecular and Translational Therapy Strategies of the Hannover Medical School (MHH) has now detected certain biomarkers in severely ill COVID-19 patients that are typically found in inflammatory processes and in patients with heart disease and offer possible new therapeutic approaches. The study, led by Institute Director Professor Dr. Dr. Thomas Thum and Dr. Christian Bär, was funded by the German Heart Foundation and published in the European Journal of Heart Failure. First authors are Ankita Garg, PhD, Dr Benjamin Seeliger and Dr Anselm Derda.
MicroRNAs identified as markers of cardiovascular damage
"We hypothesised that so-called non-coding microRNAs, which do not carry blueprints for genetic information, play an essential regulatory role in the exuberant immune response and subsequent remodelling of connective tissue in the lungs and heart. We already knew that these microRNAs are also detectable in the blood," explains Professor Thum. In cooperation with the MHH department of cardiology and angiology as well as the department of pneumology, the research team examined blood samples from 38 COVID-19 patients who were receiving intensive medical treatment and ventilation. "Therefore we focused on various sensitive microRNA markers for cardiovascular damage and analysed how high their concentration was in the blood serum," the institute director says.
For comparison, the study also examined the blood of flu patients with Acute Respiratory Distress Syndrome (ARDS), who also had to receive intensive medical treatment and ventilation, as well as blood samples from a healthy control group. The result: Compared to the healthy group, the concentration of microRNA markers in the blood serum of the severely ill COVID-19 patients was significantly increased. However, it also differed significantly from the values of the severely ill, also mechanically ventilated influenza ARDS patients.
The evidence that the heart is also affected by SARS-CoV-2 infections may have implications for the treatment of the patients. "According to our estimation, the heart function of COVID-19 patients would have to be observed in the long term course," says cardiologist Thum. In addition, the research team now wants to investigate whether the biomarkers can also be used to estimate prognosis for the course of the disease and recovery. The microRNAs could also provide approaches for new therapies.
SARS-CoV-2 mutated: What we know about the Corona variants

In recent weeks, there have been repeated reports of new variants of the previously known coronavirus from Great Britain, South Africa and Japan. Should we be afraid of these mutations? Prof Dr Matthias Stoll, MHH infectiologist, explains.
Status: 15. January 2021
Why are these mutations currently attracting so much attention?
Prof. Stoll: The press reports about variants of the SARS-CoV-2 virus suggest that this phenomenon is something new, unexpected or threatening for SARS-CoV-2. What is new, however, is simply the high level of public awareness since the first press announcements about a new variant that has been increasingly seen in the south-east of the UK. This increased perception is based on two features: Firstly, sequencing of genetic material from SARS-CoV-2 isolates - which was based solely on scientific grounds - had been carried out about 100 times more frequently in the UK than in Germany and other regions up to that point. This explains the - incidentally false - perception that it would be a SARS-CoV-2 variant only present in Great Britain or - also false - found there for the first time. Secondly, the variant was announced very effectively in the press by British Prime Minister Boris Johnson, combined with the claim that it would be a more contagious and dangerous virus than the other SARS-CoV-2 variants - and that this variant would explain the rampant infection figures in the UK. At least this last point cannot be true. For one thing, only a small proportion of COVID-19 cases are caused by this so-called variant B 1.1.7 in the UK, and for another, the wave of infections there is mainly due to public health measures.
Isolated cases of these mutations have now also been registered in Germany. Should this worry us?
Prof. Stoll: Cases of B 1.1.7 had already been described in other countries well before it appeared in the UK. One of the first cases described in Germany was treated in November at the MHH on one of the COVID-19 wards and his virus was sequenced by the MHH virology department. Its chain of infection could be traced back to Great Britain. Serious scientific investigations are currently underway in various places to clarify whether the virus is actually more contagious or more dangerous.
How do these mutations occur? Will there be more mutations?
Prof. Stoll: The success model of SARS-CoV-2 and most other viruses in the early phases of a pandemic or epidemic is based on spreading as quickly as possible and optimising its adaptation to the host with a particularly high multiplication and mutation rate. As early as May 2020 - i.e. a few months after the first cases in Wu Han - it was described that worldwide - and partly simultaneously - a mutation of the amino acid at position 614 (D614G) of the SARS-CoV-2 spike protein occurred and partially completely displaced the original virus within barely three months. The researchers were able to show that the 614G variant replicated faster than its viral ancestor with D614.
How do the three variants differ?
Prof. Stoll: All variants have mutations in the spike protein. The spike protein is the tip of the "crown spikes" that gave the "Corona" virus its name. With this protein, the virus binds to our body cells via the ACE2 receptor present there.
I don't know many more details about the Japanese variant, which has only been found in four people so far. The variants from South Africa and Great Britain have a lot in common: both variants have a mutation at amino acid 501. This mutation (N501Y) was already described half a year ago in Beijing and had attracted attention in animal experiments because it was the only variant of SARS-CoV2 that could also infect experimental mice. The idea that the virus could decisively change its contagiousness at this point is therefore obvious. All other statements about an increased risk of disease or death are so far completely speculative.
Are the mutations more dangerous than the known coronavirus?
Prof. Stoll: We don't know yet. Scientific research is in full swing, but it will take some time. Our society is finding it increasingly difficult to tolerate this state of uncertainty in times of delay-free digital communication. I am somewhat unhappy that such far-reaching and dubious speculation is currently taking place. It is quite possible that the mutations have no significance at all for the intensity of the disease.
If this is not the case, we should ask ourselves why the mutations in a pandemic that has been going on for a year should now (only) bring an inevitable catastrophic turn to mass illness and more severe courses. The experience from the co-evolution of (new) pathogen and host is generally like this: The pathogen manages to infect its host more and more effectively. There is evidence of this with D614G and N501Y. At the same time, however, it is necessary for the virus to keep its host infectious as effectively as possible and for as long as possible. This, however, means precisely the opposite of severe diseases, which are characterised by strong defence reactions and consequent lung failure and premature death. Both sides thus find a - more or less - "peaceful" coexistence. This assumption could be supported by observations that the new virus variants possibly spread more quickly among children and adolescents than the previously predominant variants. Young people have also been comparatively less severely ill with SARS-CoV2 than older people. So what we are seeing may be the beginning of a good development for us humans.
What does the occurrence of mutations mean for vaccination protection, do we need new vaccines?
Prof. Stoll: So far, we can be confident that the vaccines currently in use also cover the virus variants currently reported in the press, because these lead to very many immune responses against presumably all important antigen sections of the spike protein. It is then not a matter of a single amino acid exchange. If the vaccines should lose their effectiveness due to more and more mutations, the mRNA vaccines in particular offer the comparatively simple possibility of adapting the vaccine. The technique of mRNA vaccination has been developed and optimised precisely for this purpose - the constant adaptation to changing tumour antigens.
MHH starts Corona vaccination of employees

Vaccination centre has started work / Even those vaccinated must strictly adhere to hygiene rules
Status: 07 January 2021
On Thursday morning, the time had come: Hannover Medical School (MHH) started to vaccinate its employees against the SARS-CoV-2 virus. Dr Thomas Rebe, head of the company medical service, was the first MHH employee to vaccinate Farah Demir, a nurse in intensive care unit 14 for COVID 19 patients. The second to receive a vaccination was Martina Toussaint, head of nursing at the Central Emergency Department, with the COVID 19 mRNA vaccine from Biontech/Pfizer. MHH President Professor Dr Michael Manns is glad that the vaccinations could start today: "This is a good motivation for the further commitment to our COVID-19 patients - but also for all other patients at MHH."
"I'm thrilled that the vaccinations are already starting," said intensive care nurse Farah Demir, "I actually didn't expect it until later." Her colleague Martina Toussaint from the Central Emergency Department is also happy about the vaccination start. "The willingness to vaccinate is very high in the emergency department team," she said, "because we see the consequences of the disease in our patients."
MHH had received a shipment of 975 doses of the vaccine, with the trade name Comirnaty, on Wednesday morning. Pneumologist and acting vice-president Professor Dr Tobias Welte explained that in allocating the vaccine, MHH strictly adheres to the prioritisation plan as stipulated by the Federal Ministry of Health. "The first to be vaccinated are employees with the highest priority, i.e. colleagues who deal with COVID-19 sufferers first." Welte stressed that "this is a safe vaccine", but that vaccination is voluntary.
The MHH has established its own vaccination centre. The Centre for Information Management has developed its own app to handle the vaccinations. Today, Thursday, and Friday, 50 employees each will be vaccinated first, and the other doses of the vaccine will be administered next week.
Professor Welte reminded all those vaccinated to continue to strictly observe all hygiene rules. "The first vaccination only offers a very low level of protection. In addition, we currently do not know whether vaccinated people can also spread the virus - any studies on this are still lacking," said the pneumologist.
Corona vaccine arrives at the MHH

Vaccination centre starts work on thursday / Even vaccinated patients must strictly observe hygiene rules
Status: January 6 2021
It was an inconspicuous package that arrived well-guarded at Hannover Medical School (MHH) on Wednesday morning. The contents were 975 vaccine doses of the COVID-19 mRNA vaccine from Biontech/Pfizer. The head of the MHH pharmacy, Dr Heike Alz, accepted the precious cargo with her colleague specialist logistician Kai-Marcus Negelen. "I am glad that the first employees of the university can already be vaccinated tomorrow, a good motivation for the further commitment to our COVID-19 patients - but also for all other patients of the MHH," emphasised MHH President Professor Dr. Michael Manns.
The pneumologist and acting vice-president Professor Dr. Tobias Welte adds that this will be done strictly according to the prioritisation plan in accordance with the specifications of the Federal Ministry of Health. "First of all, employees with the highest priority are vaccinated, i.e. colleagues who have to deal with COVID-19 patients. These are mainly employees from the emergency room and intensive care units who want to receive such a vaccination." The MHH has set up its own vaccination centre, he said. Dr Bastian Ringe from the MHH's COVID-19 task force explains that the first 50 employees will be vaccinated on Thursday and Friday respectively, and the other doses of the vaccine, with the trade name Comirnaty, will be vaccinated next week.
Professor Welte reminds all those vaccinated to continue to strictly observe all hygiene rules. "The first vaccination only offers a very low level of protection. In addition, we currently do not know whether vaccinated people can also spread the virus - any studies on this are still lacking," says the pneumologist.
Corona pandemic: MHH is a safe place to be
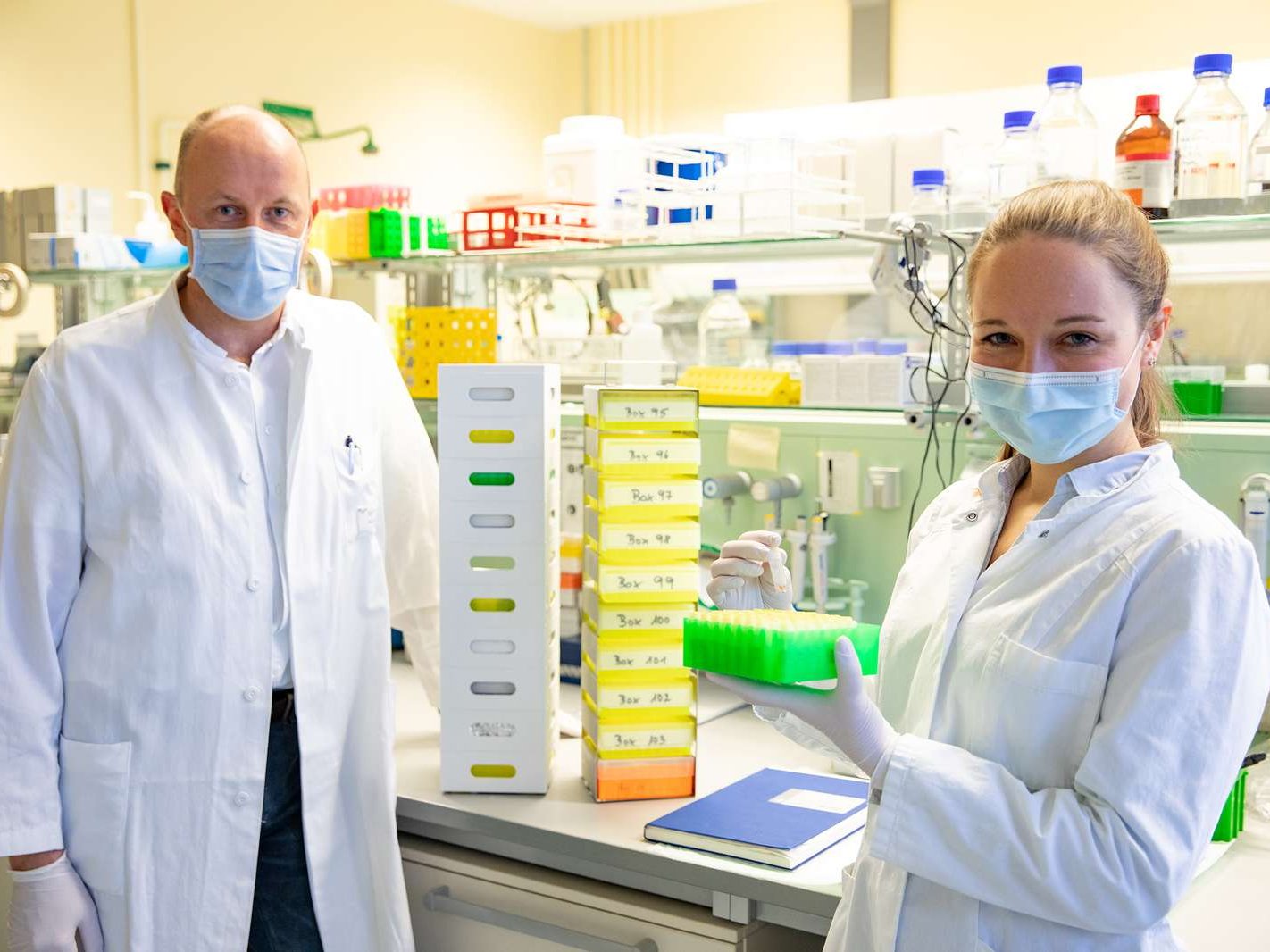
CoCo study: Next step is to investigate immune response after Corona vaccination.
Status: January 4 2021
Since the start of the Corona pandemic in Germany in March 2020, a research team from the MHH Department of Rheumatology and Immunology has been investigating in the CoCo (COVID-19 Contact) study how frequently SARS-CoV-2 infection has occurred among healthcare personnel. This was done by testing blood for antibodies to SARS-CoV-2, which indicates an infection has occurred. "Above all, we wanted to know how many participants had fallen ill without noticing it," says study leader Professor Dr Georg Behrens.
The reassuring results: There were far fewer infected than feared. Antibodies against SARS-CoV-2 could only be detected in about one per cent - a very low infection rate compared to the population of the Hannover Region. Only two of the more than 1,250 people tested had become infected by November without knowing it. Therefore, the fear of infecting oneself in the clinic is largely unfounded. And this is not only due to the relatively low number of COVID-19 patients so far. The clinic staff themselves also make a decisive contribution by obviously working responsibly and observing the hygiene regulations.
More than 1,000 employees participate in the CoCo study
The MHH is one of the first institutions nationwide to regularly test doctors and nurses from routine clinical and emergency care of COVID-19 patients. "We tested blood samples from more than 200 participants weekly at first, then monthly, and at the same time recorded possible symptoms with the help of questionnaires," explains Anne Cossmann, a doctoral student at the clinic and one of the organisers of the study. A logistical feat, because due to the distance rules, the participants could not be ordered centrally to take blood samples. "But since they are all medically trained, fortunately they took the blood samples themselves, we had, so to speak, all kinds of little study centres on campus," says study director Behrens. In the meantime, another 1,000 volunteers have been recruited and will be tested every six months. The interest in the CoCo study is enormous. "We are grateful for the willingness to participate, but unfortunately we cannot include any more interested people," says Professor Behrens.
The next step is to investigate vaccination protection
Now the study is entering a new phase, as vaccinations against SARS-CoV-2 will start soon. The next goal is to investigate the immune response triggered by this. "We have sent out questionnaires in advance to our participants about their possible participation in the vaccination. Based on the responses, we assume that 70 to 80 percent will be immunised against the Corona virus," estimates Professor Behrens. This leads to the question of how strongly the vaccinees respond to the vaccine, how many antibodies they form and how long the vaccine protection lasts. But participants who do not want to be vaccinated will also continue to be tested within the CoCo study. They will find out the results on a website set up especially for the clinical trial. "The site is a kind of communication platform for news, background information and diagrams," explains Anne Cossmann. The participants can log in with a personal password, ask questions and retrieve their study results - all pseudonymised and in compliance with data protection regulations.
What we now know about the COVID-19 long term sequences

Status: December 15 2020
Prof. Dr. Tobias Welte, pulmonologist and acting vice-president of the MHH, clarifies the status regarding the long-term consequences of COVID-19 diseases.
What are the complaints of those affected?
In the post-COVID-19 outpatient clinic of the MHH there are many people who suffer from symptoms after surviving an illness. But one must differentiate here. On the one hand, there are people who have been treated in the intensive care unit of the hospital due to a serious COVID-19 disease. These people do not leave the hospital without complaints because they sometimes had to be ventilated for weeks. But there are also patients who were only slightly ill and who report to the COVID outpatient clinic with complaints afterwards.
The complaints can also be subdivided. On the one hand, people complain about shortness of breath. The MHH physicians find that they have changes in the lungs, but also in the heart. For example, the pumping capacity of the heart muscle or the heart rhythm has changed. But these are the fewest cases. In addition, patients with chronic diseases - especially of the kidney and liver - can suffer permanent deterioration. Many more patients, however, have the so-called fatigue syndrome, a kind of fatigue syndrome. This manifests itself in exhaustion, insomnia, concentration problems, reduced performance and lack of drive.
How can these complaints be treated?
The organic diseases of the lungs and heart, for example, can be specially treated. There is no special therapy for the neurological symptoms - the fatigue syndrome and also loss of the sense of taste and smell. At the MHH, we try to provide targeted help with physiotherapy, respiratory therapy and neurocognitive training, depending on the type of complaints. If the sense of taste or smell is lost, training of these senses is also possible.
Those affected regularly visit the post-COVID outpatient clinic for weeks and months, and the doctors observe very clearly that the complaints diminish over the course of time and that people are getting better and better.
Is there an explanation for these neurological symptoms?
The fatigue syndrome is not new. It is known in connection with other infectious diseases such as Pfeiffer's glandular fever, in neurological diseases and also in the lung area. Presumably, the disturbance of the nerve muscle tissue plays a role in triggering this syndrome.
The olfactory disorder, on the other hand, has already been very well analyzed. Here, the corona viruses attack the olfactory cells, i.e. the cells responsible for the sense of smell. The damage can have different effects: If only the cells are affected, the disorder quickly recedes. However, if the supplying nerve is affected, it can take a very long time until the sense of smell is functioning again.
How many people suffer from long-term effects?
A rough estimate is that two to three percent of COVID-19 sufferers develop a pronounced post-COVID syndrome. There will probably be far more people who have slight limitations after the disease. But these people do not report it because they do not suffer from it in everyday life.
In principle, anyone who has been ill once can develop such long-term consequences. Whether the individual notices it very strongly or not at all also depends on his or her original physical condition and fitness before the illness. A competitive athlete notices even a slight limitation of his fitness very quickly and clearly. Someone who is rather motionless in everyday life does not notice the consequences so quickly. This could be the reason why younger, fit people in particular tend to suffer more, although they do not fall ill more often.
Vaccine against Corona: What we currently know
Status: December 7 2020
MHH infectiologist Professor Dr. Matthias Stoll explains the current status of the corona vaccine.
Among the promising vaccine types are live and dead vaccines, vector vaccines and recently also mRNA vaccines. What are the differences?
Prof. Stoll: The basic principle of any vaccination is that a specific immune response directed against the antigen is specifically induced in the body by molecular structures foreign to the body ("foreign antigens"). After this learning phase of the immune system, the antigen can later be called up quickly and effectively - for example, if the foreign antigen is recognized on an infectious agent and prevents the respective disease from breaking out.
In the past, dead vaccines consisted of completely killed pathogens, hence the name dead vaccine. Nowadays, only partial components (so-called split vaccines or subunit vaccines) or artificial, genetically engineered antigens of specific pathogens are usually used instead. All the variants mentioned are combined as inactivated vaccines in order to make it clear that the pathogen(s) (components) in these vaccines cannot multiply by themselves. Inactivated vaccines stimulate the body's own defense system, especially to produce antibodies.
Live vaccines consist of pathogens that are capable of replication but are attenuated. These do not trigger the disease itself, but can occasionally cause a temporary, harmless "vaccination disease".
Vector vaccines belong to the group of live vaccines and consist of pathogens that are harmless to humans and which carry antigens of the pathogen through targeted genetic modification. The carrier virus - also known as vector virus - modified in this way functions more or less like a Trojan horse, with which the blueprint for an immune response against an infectious disease is offered to the center of the immune defense for replication.
m-RNA vaccines are basically a further development and minimization of the Trojan horse principle of a vector vaccine: the vector virus, which is not necessary for the actual immunization, is dispensed with and instead only a genetically engineered genetic information of pathogen antigen(s) is introduced for vaccination. The vaccinated person's own cells are temporarily stimulated to produce this foreign antigen and present it to the immune system in a particularly advantageous way. This results in a variety of specific immune responses. A further advantage is that the m-RNA is completely degraded after the work is done and that it is not possible for the human cells to convert genetic information from the m-RNA into the genetic DNA code of our own genetic material. This increases the safety of the vaccination concept because the process artificially set in motion by the vaccination cannot take on a life of its own.
How long does it take to become immune after a vaccination?
Prof. Stoll: A specific immune response - the desired consequence of a vaccination - gradually gets going after just a few days, but it takes about two weeks or a little more until it reaches the desired level. Almost all vaccinations developed against COVID-19 disease then take a second step, however, because a booster vaccination must be given at intervals of three weeks to two months so that the vaccination protection is higher on the one hand and lasts much longer on the other. This means that the COVID vaccinations do not develop their full effect until at least four to six weeks after the first dose.
Does every vaccine make you immune in the same way?
Prof. Stoll: Indeed, there are currently about 50 different corona vaccines in clinical trials worldwide. Each vaccine elicits a specific immune response, but the associated effective protection against infection depends on several factors:
- The selection of a suitable vaccine that triggers the immune reactions that are decisive for protection as precisely as possible and stores these specific immune responses in the long-term memory of our immune system.
- The type of vaccine, e.g. as live vaccine, dead vaccine or RNA vaccine Each vaccination principle leads to different variants of the immune defense. Live vaccines and RNA vaccines are particularly well able to induce several variants of the specific immune defense simultaneously, i.e. not only an antibody response but also a cellular immune response.
-
Not only the vaccine plays a role, but also factors in the person to be vaccinated. Old age, male sex, certain diseases and the use of certain drugs are some of the factors that are associated with a less pronounced immune response. However, we try to design the vaccines in such a way that even under such conditions a sufficient immune response is still produced.
How long does the vaccination effect last?
Prof. Stoll: For COVID-19, we do not yet know because there are no long-term observations. Unfortunately, the immune reactions against SARS-CoV-2 seem to decrease more rapidly than for many other infections. Whether the immune protection of a vaccination also decreases more rapidly to the same extent is still unknown. Therefore, it could be that regular booster vaccinations might be necessary, as is the case with the flu or tetanus vaccination.
Who should be vaccinated?
Prof. Stoll: As many people as possible in order to achieve a worldwide herd immunity, which in the ideal case would cause SARS-CoV-2 to disappear completely from humanity again. However, at first there will be no vaccine available for everyone, nor will it be possible to vaccinate all 80 million Germans in a few days or weeks. For this reason, the National Ethics Council and other specialized institutions have recommended that priority be given to vaccinating those who have a greatly increased risk of contracting COVID-19 - as well as people in the health care system and employees in so-called systemically important professions, such as the police and fire department. Employees* at the MHH are among the first to be vaccinated.
Should high-risk patients with weakened immune systems also be vaccinated?
Prof. Stoll: Yes! Exactly such people are among the people who should be vaccinated first. In individual cases, however, it must be clarified when the most favorable time for vaccination is during the course of the disease or within the framework of an ongoing immunodeficient therapy. In the case of very severe immune deficiencies, the question of whether the vaccination could cause a risk would also have to be clarified with the treating physician.
Should also people who were already infected with the virus be vaccinated?
Prof. Stoll: So far I am not aware that people who already had COVID-19 were excluded from the vaccination. Such a concept would not make sense either, because it is known that the naturally acquired immune response of these so-called convalescents very often decreased rapidly again.
How great is the risk of problematic side effects?
Prof. Stoll: The two m-RNA vaccines from the companies Biontech/Pfizer and Moderna are said to be quite well tolerated - according to the manufacturers' information and also according to statements by independent study observer boards. Main side effects were rather mild - at least not life-threatening - and temporary, such as headaches and/or reactions at the injection site. On the other hand, data on possible long-term side effects are not yet available, as these are accelerated approvals. However, the potentially increased risk due to the lack of long-term data is taken into account by obligatory and comparatively costly observation and documentation of adverse events in all persons vaccinated with the new vaccines.
What percentage of the population must be vaccinated to stop the spread of the virus?
Prof. Stoll: To achieve herd immunity against the SARS-CoV-2 virus, at least 70 to 75 percent of the population must be immune. These percentages are simply calculated from the basic reproduction number (R0) of the virus, which is given by the Robert Koch Institute and in several published meta-analyses* between 3.3 and 3.8. In a recent representative survey conducted by Barmer Krankenkasse at the end of November 2020, the willingness to be vaccinated against COVID-19 for adult Germans was only 53 percent, while for Lower Saxony it was 56 percent. Unfortunately, however, with these low vaccination rates, the hoped-for transfer to a world without lockdown and AHA rules would not be achievable in Germany.
The questions asked: Vanessa Meyer
*(i) Lin YF et al. Frontiers in Medicine. 2020;7:321; (ii) Liu Y et al. Journal of travel medicine. 2020. 53; (iii) Alimohamadi Y, et al. Journal of preventive medicine and public health. 2020;53(3):151-7.
MHH starts COVID-19 therapy study with blood plasma from convalescents

Status: November 17, 2020
There is still no really promising drug against COVID-19. One option is the treatment with blood plasma of people who have already survived this disease - with so-called convalescent plasma. Antibodies against the virus contained in blood serum could support the immune defence of infected persons in their fight against SARS-CoV-2. Now a new clinical study is to clarify how well this passive immunization actually works. Under the direction of Professor Dr. Rainer Blasczyk, Head of the Institute for Transfusion Medicine and Transplant Engineering at Hannover Medical School (MHH), researchers from the MHH, the clinics in Dortmund, Krefeld, Magdeburg and Essen as well as the Siloah Hospital in Hannover are investigating whether the therapeutic transmission of antibodies against SARS-CoV-2 can prevent severe courses of COVID-19 disease. The multi-center study, entitled COMET, starts this Tuesday at the MHH and is funded by the German Federal Ministry of Health (BMG) with approximately 3.34 million Euros.
Preventing severe disease progression
Although convalescent plasma is already being used in clinics against COVID-19 - due to the special situation in times of a pandemic, an exception is provided for in the German Medicines Act. However, there is still no proof of efficacy for this form of therapy. This is now to be provided by clinical studies. Two of these are already underway, but are investigating plasma administration in critically ill patients. In contrast, 340 COVID-19 patients between the ages of 18 and 75 years, who have a rather mild course of disease, are participating in the COMET study: Although they need to be treated in a hospital, they do not yet require ventilation. Passive immunization with the donated pathogen-specific antibodies could thus prevent lighter COVID-19 patients from having to be transferred to the intensive care unit during their hospital stay. "We believe that the earlier we use adoptive immunotherapy, the better," says Professor Blasczyk. The transfusion physician is therefore convinced that prophylactic treatment - for example for non-infected high-risk patients - could even prevent the disease completely.
Donor plasma is being closely examined
The study participants are divided into two groups. One group will receive 250 milliliters of donor plasma on two consecutive days, the other group will not receive plasma as a comparison group. In order to ensure that the plasmas contain sufficient anti-SARS-CoV-2 active antibodies on the one hand and no potentially harmful substances on the other, the donor plasma is first tested in the laboratories at the MHH Institute of Virology and TWINCORE. "Plasma has two advantages: It is safe and is available within a short time", emphasises Professor Blasczyk. The COMET study runs until the end of next year. However, the transfusion physician hopes to be able to present results much earlier.
For plasma donations COVID-19-Genesene can turn to Institut for transfusion medicine and transplant engineering under RKP-Spende@mh-hannover.de.
Information on the COMET study can be found here.
MHH is looking for volunteers aged 60+ for Corona study

Tuberculosis vaccine is intended to strengthen the immune system against the corona virus in older people.
Status: November 05, 2020
A vaccine against tuberculosis could help to achieve a stage victory against the corona virus. The MHH is therefore increasingly looking for people over 60 years of age to be vaccinated with the so-called immune booster VPM 1002. The preparation is intended to strengthen the immune system in its fight against the Sars-CoV-2 pathogen. "VPM 1002 is the genetically improved variant of a vaccine that is decades old and is used in many countries to fight the tuberculosis pathogen," says Professor Dr. Christoph Schindler from the Hannover Medical School (MHH), head of the CRC Core Facility at the Clinical Research Center Hannover. Because the vaccine apparently not only helps against the Tuberculosis bacterium but also improves the immune response in general, it could also strengthen the defense against the corona virus. "In the ideal case, the vaccination reduces the probability of contracting corona virus disease," explains Professor Schindler. Interested persons can contact us at: Telephone (0511)-5350 8333 (recruitment telephone) or by e-mail at: CRC.Studienteilnahme@mh-hannover.de
SARS-CoV-2: How many neutralizing antibodies are needed for protection?

Status: November 05, 2020
Infections with the coronavirus SARS-CoV-2 can progress in very different ways: While some people have no symptoms, others fall seriously ill. An important question that often arises after surviving an infection is the extent to which neutralizing antibodies against the virus have been produced, as only these can protect the body from re-infection.
To detect neutralizing antibodies, infectious viruses, living cells and laboratories with a high safety standard are usually required. Due to the very high requirements of this test, only very limited blood samples from convalescent patients can be tested for the presence of neutralizing antibodies in blood serum. "To change this, we have developed a very simple and rapid procedure that requires only two proteins that are important for the infection process: The spike protein of the virus and the protein ACE2 of the cell. If the binding of the spike protein to ACE2 is suppressed by serum antibodies, these antibodies are also able to prevent the infection of cells with the virus," says Dr. Berislav Bosnjak from the Institute of Immunology at the Hannover Medical School (MHH). He is first author of the study now published in the journal Cellular and Molecular Immunology.
New test can be further developed for the clinic
"With the help of the test developed by us it is now possible to examine a large number of patients over a longer period of time in clinical studies and to determine how long these so important antibodies are present in the blood", emphasizes Professor Dr. Reinhold Foerster, head of the MHH Institute of Immunology and senior author of the study. The new method is still only available for research. However, it could potentially be adapted so that it can be used for routine tests in the future.
With both the previous and the new method, the team was able to show that about ten percent of SARS-CoV-2 infected persons had no protective antibodies in their blood. This primarily affected infected persons who showed only mild symptoms and were only ill for a short time. On the other hand, the patients developed many antibodies that had stronger symptoms and were ill for longer periods of time. "It is still unclear how much neutralizing antibody is needed to protect convalescents from re-infection. But with the test now available, it will be possible to answer this important question more quickly," says Professor Förster.
Other staff members of the MHH Institute of Immunology, the Institute of Virology and the Institute of Transfusion Medicine and Transplant Engineering were involved in the study. Teams of the Clinic for Rheumatology and Immunology as well as the Clinic for Pneumology and the German Primate Center in Göttingen also participated.
The research project "Low serum neutralizing anti-SARS-CoV-2 S antibody levels in mildly affected COVID-19 convalescent patients revealed by two different detection methods" was funded by the Corona Research Funding Program of Lower Saxony, the Cluster of Excellence RESIST and the Collaborative Research Center SFB 900 of the German Research Foundation.
Keyword: Neutralizing antibodies
Of the antibodies that people have in their blood after successfully surviving an infection with SARS-CoV-2, the neutralizing antibodies are particularly effective. They are a particularly important group of antibodies because they dock to the virus and prevent the virus from entering and multiplying in human cells. Neutralizing antibodies can therefore switch off the virus.
You can find the original paper here.
Corona tests and basics of therapy: MHH researches with
Together against Corona: The Hannover Medical School is involved in eight projects of the National Network of University Medicine.
Status: October 23, 2020
Good research needs good networks, especially in times of global challenges. In the fight against the coronavirus SARS-CoV-2, this is being done in Germany with the "National Network of University Medicine on Covid-19". A network of all German university hospitals is addressing urgent research topics and bundling cross-clinical research activities in 13 projects to tackle the corona pandemic. The Hannover Medical School (MHH) is involved in eight projects. "I am pleased that the MHH is able to contribute its proven research expertise and experience in the treatment of Covid-19 patients and thus contribute to the best possible care for patients throughout Germany," said MHH President Professor Dr. Michael Manns. The Federal Ministry of Education and Research (BMBF) is supporting the research activities in the network with a total of 150 million euros.
The MHH is involved in the following eight network projects of the National Network of University Medicine:
B-FAST - "Nationwide Research Network Applied Surveillance and Testing
Surveillance comprises the observation, analysis, interpretation and reporting of health data. The corona pandemic shows that different testing and surveillance strategies are needed for the entire population, schools and daycare centers, potential risk areas and clinics. B-Fast is developing a platform where such strategies can be tested. To do so, it brings together different analyses and assessments. In this way it supports strategies that not only help in the acute crisis, but can also be transferred to future pandemics.
COVIM - "Determination and use of SARS-CoV-2 immunity
In the project, numerous university hospitals cooperate to combine immunological data from population studies and the investigation of Covid-19 genesis and to generate new scientific knowledge about immunity against SARS-CoV-2. Furthermore, it shall be investigated how the immunity can be transferred to other persons and used for new therapeutic approaches. COVIM closely cooperates with the projects also funded in the network University Medicine, in particular with NAPKON, B-FAST and CEO-sys.
DEFEAT PANDEMIcs - "German Research Network Autopsies in Pandemics
In the project, a Germany-wide autopsy network is being established, in which data, biomaterials and findings are systematically and in a standardized way collected and brought together. This unique networking of most of the pathological, neuropathological and forensic institutes of German university hospitals as well as non-university partners will enable a deeper understanding of the disease and help to develop more effective therapeutic approaches.
EViPan - "Development, testing and implementation of regionally adaptive care structures and processes for evidence-led pandemic management coordinated by university medicine"
A national pandemic management is needed to identify and treat Covid-19 patients even faster and better in the future and to maintain optimal routine care. It also helps to prevent infections and provides an ethical and normative evaluation of care scenarios under pandemic conditions in order to be better prepared for future pandemics. As internationally networked maximum care providers and research institutions, university hospitals are at the center of regional health networks. In the project, they cooperate with the Robert Koch Institute, the public health service and the state governments in order to jointly achieve the goal.
FoDaPl - "National Research Data Platform
In this project, a nationwide uniform, data protection-compliant infrastructure for the storage of Covid-19 research data sets will be created. In this research data platform, for example, laboratory data can be made available to researchers in pseudonymized form using secure and transparent procedures. Thus, the platform will become a central source of information for various research projects dealing with the development of better treatment approaches for Covid-19.
NAPKON - "National Pandemic Cohort Network
The NAPKON project is creating the basis for a better understanding of the course of disease in Covid-19 and for research into possible therapies by bringing together clinical data, biosamples and imaging data in scientific studies. NAPKON is closely linked to the establishment of the National Research Data Platform and cooperates with the COVIM project. The studies thus made possible can, for example, provide information on the long-term consequences of covid-19 disease, even if the patients change their family doctor during treatment, for example, from the clinic to their family doctor.
PallPan - "National Strategy for Palliative Care in Pandemic Times
In this project, recommendations for action and information material are being developed on a scientific basis in order to provide the best possible care for seriously ill and dying people, even in pandemic times, and to take their concerns - and the concerns of their relatives - into account. This is the largest structured association of palliative care in a research project in Germany to date. All areas of outpatient and inpatient hospice and palliative care (general practitioners, specialists, nursing services, palliative services, homes, hospitals, hospices) are considered.
RACOON - "Radiological Cooperative Network on Covid-19 Pandemic
RACOON is the first Germany-wide radiology platform in which almost all university hospitals are involved. Here, radiographs of patients with suspected Covid-19 are brought together and related to the course of the disease. The findings are analyzed using artificial intelligence. This enables a faster and more precise diagnosis of the disease and its progression and provides a basis for decision-making in epidemiological studies, situation assessments and early warning mechanisms.
For further information on the B-FAST project, please contact Professor Dr. Dr. Michael Marschollek by phone (0511) 532-5295 or at marschollek.michael@mh-hannover.de
For further information on the COVIM project, please contact Professor Dr. Thomas Schulz by phone (0511) 532-6737 or at schulz.thomas@mh-hannover.de
Further information to the project DEFEAT PANDEMIcs receives you with professor Dr. Danny Jonigk under telephone (0511) 532-9532 or under jonigk.danny@mh-hannover.de
For further information on the EViPAN project, please contact Professor Dr. Jörg Haier by phone (0511) 532-19307 or at haier.joerg@mh-hannover.de
Further information to the project FoDaPl receives you with professor Dr. Dr. Michael Marschollek under telephone (0511) 532-5295 or under marschollek.michael@mh-hannover.de
Further information to the project NAPKON receives you with professor Dr. Thomas Illig under telephone (0511) 532-7856 or under illig.thomas@mh-hannover.de
Further information to the project PallPan receives you with professor Dr. Nils cutter under telephone (0511) 532-2744 or under schneider.nils@mh-hannover.de
Further information about the RACOON project can be obtained from Professor Dr. Frank Wacker by phone (0511) 532-3422 or under wacker.frank@mh-hannover.de
MHH researchers find possible helpers against COVID-19 infection in the heart
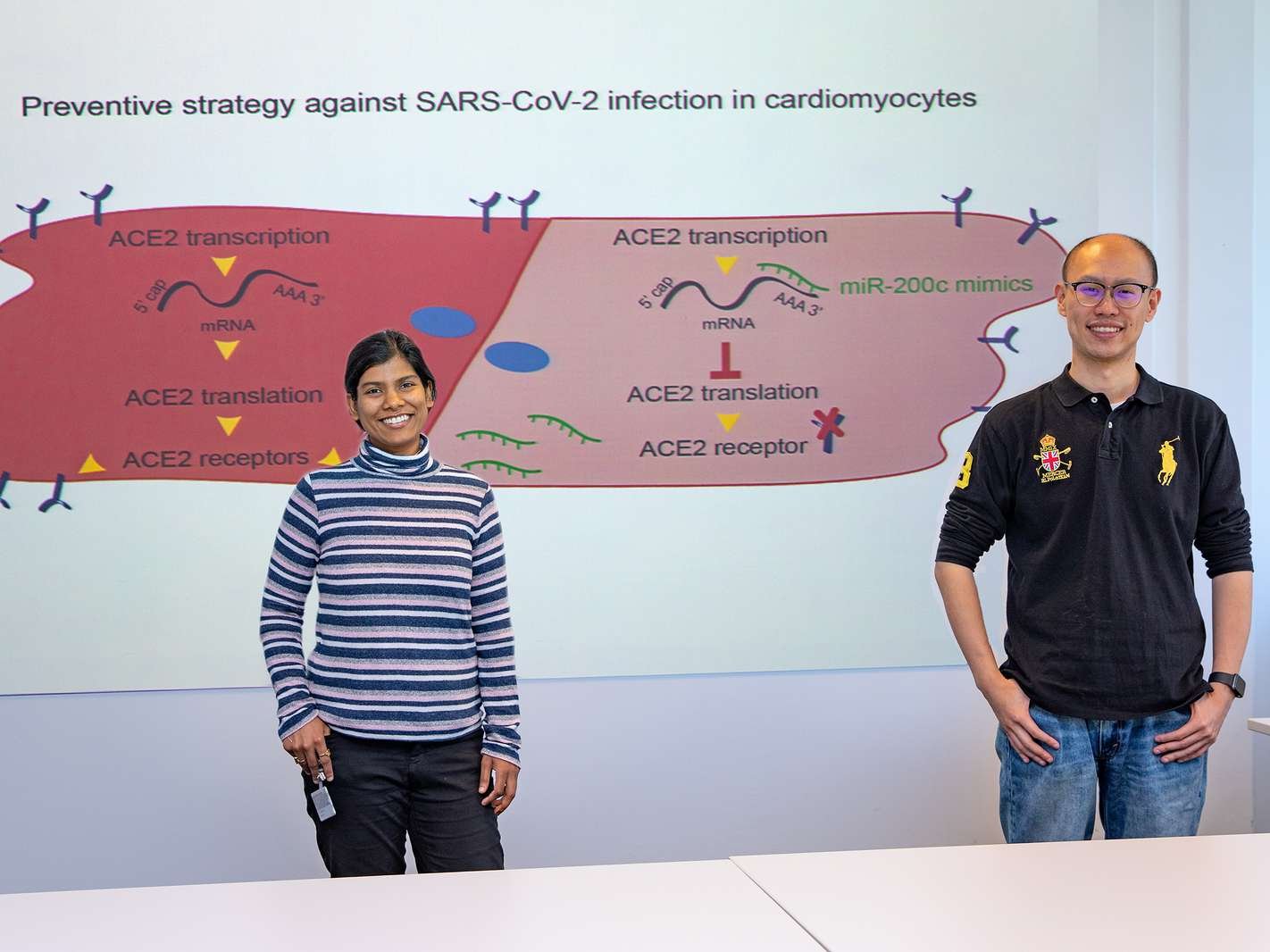
Status: October 2, 2020
Infections with bacteria and viruses are an additional burden on the cardiovascular system. This also applies to the coronavirus SARS-CoV-2, but the virus appears to cause heart damage not only in older people with underlying cardiovascular diseases. Even slightly ill younger patients can show inflammatory changes in the heart muscle or pericardium after surviving COVID-19 infection. This is caused by the angiotensin-converting enzyme 2 (ACE2). This binding site is the gateway for SARS-CoV-2 to enter the lung tissue. Because ACE2 is also found in heart muscle cells, the viruses can also attack the heart and cause massive inflammation there. A research group at the Institute for Molecular and Translational Therapeutic Strategies at Hannover Medical School (MHH) has now discovered a way to block this pathway for the coronavirus. The study under the direction of Institute Director Professor Dr. Dr. Thomas Thum Dr. Christian Bär has been published in the Journal of Molecular and Cellular Cardiology. First authors are Dongchao Lu and Shambhabi Chatterjee, PhD.
Corona viruses attack cells via ACE2 enzyme
ACE2 controls the salt and fluid levels in the body and regulates blood pressure. As one of the major receptors for SARS-CoV-2, ACE2 is also a potential target for COVID-19," said Professor Thum. His research team has been looking for ways to down-regulate the enzyme concentration and, using bioinformatics methods, has discovered a group of microRNAs that control the process. microRNAs are tiny, non-coding RNA snippets that do not implement a genetic blueprint, but can very specifically prevent the construction of individual proteins in the cell.
miR-200c downregulates ACE2 activity
"One candidate in particular, called miR-200c, was able to significantly downregulate ACE2 activity in rat heart muscle cells and in human cardiomyocytes produced from stem cells in the laboratory," said study leader Dr. Baer. In the next step, the promising results from the cell culture experiments must now be tested in living organ simulations. If the study is also successful in a mouse model, the use of miR-200c could be an important strategy in the fight against corona viruses in the future - even if an effective vaccine is available. "The pathogens causing the serious respiratory diseases SARS and MERS are also among the corona viruses that enter cells via ACE2," Professor Thum emphasizes. It is therefore not unlikely that this mechanism can also be used in a future coronavirus pandemic.
The original publication "MicroRNAs targeting the SARS-CoV-2 entry receptor ACE2 in cardiomyocytes" is available online here
Virtual visit to the MHH-Kreißsaal

Status: August 25, 2020
MHH goes new ways to inform pregnant women in times of Corona / Every Monday a live broadcast with expert discussions starts at 6.30 pm / Registration by mail
The gynaecological clinic of the Hannover Medical School (MHH) is a very popular address for pregnant women in the Hannover region. "We offer our committed and highly professional care for normal birth up to and including high-risk pregnancy," says clinic director Professor Dr. Peter Hillemanns. While prospective parents were able to visit the maternity clinic before the corona crisis, the gynecological clinic now has to find new ways to reach future mothers and fathers. Even under the clear limitations of the COVID 19 crisis, the gynecological clinic would like to give all expectant parents the opportunity to obtain information about the delivery room at the MHH through direct contact. "Therefore we are now pleased to offer the first web-based information evening for expectant parents in Hanover", Nina Meier, midwife in the delivery room. "We want to show the parents that they are not alone with all their questions.
Ask questions directly to the experts
Every Monday at 6.30 p.m. expectant parents can inform themselves about topics concerning pregnancy and birth at the MHH in a live broadcast. In addition, they have the opportunity to ask questions directly to the MHH experts after the general introduction and to talk to them.
Interested parties can obtain the access data via an informal e-mail to geburtshilfe.infoabend@mh-hannover.de. The live broadcast via the Microsoft Teams program begins every Monday at 6:30 pm. Technical requirements are a computer with (integrated) camera, microphone and speakers or headphones. Access is also possible with a tablet or smartphone.
Further information about the MHH Maternity Hospital is also available at www.mhh.de/praenatalmedizin-und-geburtshilfe-im-perinatalzentrum.
MHH researches late effects of corona infection

Status: July 24, 2020
COVID outpatient clinic for officially recovering accompanies concerning / participant inside and participants for study searched.
Recovered, but not healthy: Some people who were ill with COVID-19 still suffer weeks and months after the acute illness from its consequences. The symptoms include tiredness, reduced physical resilience, lack of concentration, breathing problems and loss of taste or smell. "These late effects are not only seen in patients who were severely affected and were treated as inpatients, but also in those with a moderate or mild course of the disease," explains Professor Dr. Marius Hoeper, acting director of the Department of Pneumology at Hannover Medical School (MHH). In his clinic there is the COVID outpatient clinic for convalescence, where patients are accompanied after their illness. To find out more about the late effects, Professor Hoeper and his team are conducting the study "IRMI 19" (ImmunpRofile iM long-term course after COVID-19).
The COVID outpatient clinic for convalescents is available since mid-May. "There are patients who still do not feel well three or four months after the illness", explains Dr. Isabell Pink, head of the outpatient clinic. For some of them it is difficult to pursue their profession due to the complaints, even if it is "only" an office job. Many complained of shortness of breath under stress and a tightness in the chest. Among them were also patients between 21 and 50 years of age who had been completely healthy before infection with the SARS-CoV-2 virus. "Their situation is improving only very slowly," says the pneumologist. Medically, she cannot offer the patients much. "We can only advise them to listen to their body, to shift down a gear altogether and, if necessary, to apply for outpatient rehabilitation".
Half a year under observation
Nevertheless, those affected appreciate the care in the outpatient clinic. They feel safer if they are accompanied by a doctor and their condition is observed over a longer period of time. In the outpatient clinic, the experts follow the course of the disease for at least half a year. Patients are examined three times: six to eight weeks, three months and six months after acute SARS-CoV-2 infection. These include a lung function test, analysis of blood, urine and saliva, a physical examination and a stress test, and imaging diagnostics if necessary. There is close contact with other disciplines, which are consulted as required.
Little is known about the long-term consequences of coronavirus infection. However, previous research and clinical observations have shown that SARS-CoV-2 can infect practically any organ and cause damage there. "We assume that COVID-19 has a lasting effect on the immune system," explains Professor Hoeper. Through the "IRMI 19" study, he and his team hope to gain new insights into the late effects of the virus infection. "We assume that there are correlations between the observed immune phenomena and the persistent symptoms, which we would like to understand better, of course also in the hope to be able to treat them in the future". Immunoprofiles should provide information about this in the long-term course.
About 100 affected persons, who originally had only a mild COVID-19 disease but still suffer from late effects, will participate in the study. The study may also include patients who were not treated at the MHH. They can register at the COVID outpatient clinic for convalescence.
Interested persons can reach the COVID outpatient clinic for convalescents under telephone (0511) 532-5030, fax (0511) 532-18538 or e-mail: pneumologie.covid@mh-hannover.de.
Further information receives you with Dr. Isabell Pink, hospital for pneumology, under telephone (0511) 532-9314 or pink.isabell@mh-hannover.de.
T lymphocytes play an important role in the course of COVID-19
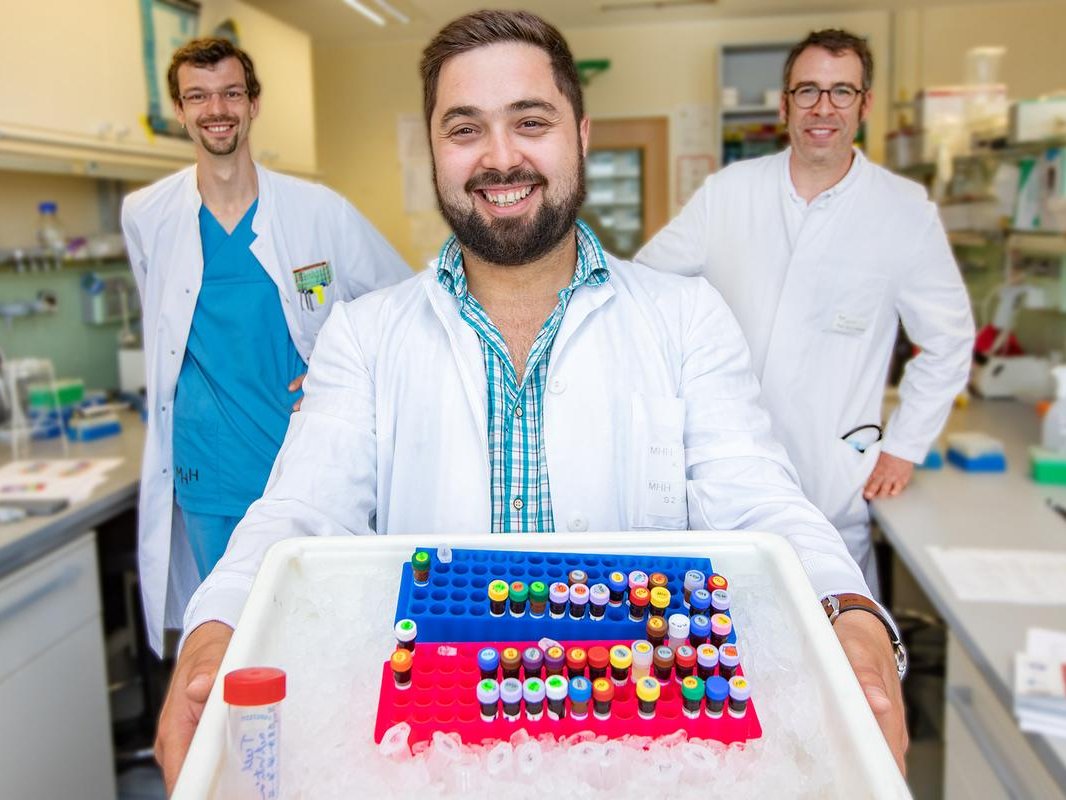
MHH research team publishes first European study of this kind in the Lancet journal "EBioMedicine
Status: 08 July 2020
Infections with the coronavirus SARS-CoV-2 can take very different courses - some people remain completely without symptoms or show a mild course of the disease. Others have to be treated in hospital. But even here there are differences between patients who need to be ventilated in intensive care units and those who are less likely to get COVID-19. A research team at the Hannover Medical School (MHH) has found out how these two groups of patients treated in hospitals differ immunologically. Led by the Institute of Immunology and the Clinic for Haematology, Haemostaseology, Oncology and Stem Cell Transplantation, the researchers studied the blood of COVID-19 patients. They found out that a certain composition of lymphocytes, which are responsible for targeted immune defence, plays an important role in the course of the disease. The research was the first European study of its kind to be published in the Lancet journal "EBioMedicine". The first author is Dr. Ivan Odak.
Number of T-lymphocytes decreases in seriously ill COVID-19 patients
"We were aware that patients with severe COVID-19 disease generally have fewer lymphocytes in their blood," says Dr. Christian Schultze-Florey, who is the co-principal investigator of the study with Professor Dr. Christian Könecke. "However, we did not know which specific subgroups and to what extent they were actually affected. Lymphocytes belong to the white blood cells and, like all blood cells, are formed in the bone marrow. They then have to go through a maturation process in the body before they can recognise and fight foreign cells such as bacteria or viruses as T or B lymphocytes. In severe cases of COVID-19 - such as patients requiring respiration - all lymphocyte subtypes were found to be reduced compared to healthy controls. This was significantly less pronounced in mild COVID-19 patients.
"Another groundbreaking finding was that COVID-19 patients with mild disease had more effector T-cells already at hospital admission than patients with a severe course," Professor Könecke explains. Effector T-cells are particularly activated T-cells that either destroy diseased cells directly or alarm the immune system with messenger substances and thus attract additional immune cells. The researchers also found differences in the course of COVID-19 disease. If patients recover from infection with SARS-CoV-2 and their health improves, the number of effector cells in the blood also increases significantly. Memory cells, which are a special form of T-cells that recognise pathogens during a renewed infection and can therefore fight them more quickly, can also be detected more strongly again during recovery. If the disease does not improve, however, there is no such increase.
More targeted diagnosis and more effective treatment possible
"The T-cell immune response seems to play a crucial role in COVID-19," says Professor Förster, head of the Institute of Immunology. The general decrease in lymphocyte subtypes and effector T cells could therefore serve as a biomarker to assess the severity of the disease at an early stage by measuring the immune status. "This is important because some patients initially appear clinically stable when they are admitted to hospital, but a severe COVID-19 course occurs a little later," emphasises study leader Schultze-Florey. These patients could be treated faster and more effectively through a targeted diagnosis. The course of treatment could also possibly be predicted with the help of T-cell markers. This would make it possible to check during treatment whether patients respond and their state of health is likely to improve.
The research project "Reappearance of Effector T Cells Is Associated With Recovery from COVID-19" was funded by the Corona Research Funding Programme of the state of Lower Saxony, the "RESIST" cluster of excellence and the Collaborative Research Centre (SFB) 900 of the German Research Foundation.
For further information, please contact Dr. Christian Schultze-Florey at phone (0511) 532-9725 or schultze-florey.christian@mh-hannover.de.
The original publication is available online at https://authors.elsevier.com/sd/article/S2352396420302607.